Karrie Wallace, Education Services Clinical Lead, Spirit Health, explains the elements that comprise diabetes education & how education at an early stage can have a significant impact on health outcomes & NHS resources
Diabetes accounts for 10% of the total NHS expenditure in England and Wales. The number of patients diagnosed with diabetes increases year on year – and 92% of people with diabetes have type 2 diabetes. Therefore, having access to diabetes education remains an NHS priority.
Nationally, 80% of the costs of diabetes are associated with the long-term complications of poor health management, particularly glycaemic control and excess weight. The United Kingdom Prospective Diabetes Study, which looked at type 2 diabetes outcomes, outlines the correlation between a lack of treatment for diabetes and other long-term health problems, including heart disease.
The financial burden of diabetes-related expenditure can be reduced if patients are provided with a service to understand their condition and how to manage their diabetes. Here, I explain the elements that comprise diabetes education, and how education at an early stage can have a significant impact on health outcomes and NHS resources.
Uptake of structured diabetes education
The National Institute for Health and Care Excellence (NICE) recommends that people with type 2 diabetes should have access to structured diabetes education (SDE), with SDE courses able to help motivate patients with diabetes to improve their knowledge and skills, enabling them to better self-manage their condition.
Despite all newly diagnosed patients being offered a place on an SDE programme, uptake can be low. The National Diabetes Audit demonstrated that just over 15% of those newly diagnosed with diabetes accessed SDE in England (while also acknowledging that SDE attendance is often under-reported). Overall, it is believed that uptake is under 20% nationally, highlighting the poor national takeup rate of SDE. The need for a new approach is clear.
Changing diabetes education
As a nation, we have embraced new levels of flexibility and digitisation in the last two years. Similar models need to be brought to diabetes education, providing access in a way that fits in with patients’ lives – be that as a fully managed service, which can be delivered locally and at convenient times across a variety of locations, including virtual self-service education, for improved uptake.
When choosing a provider, key considerations include whether they have been externally validated against the NICE criteria or are certified according to the QISMET Diabetes Self-Management Education quality standard. Programmes should consist of a structured curriculum that encourages practical involvement of participants, along with the use of problem-solving models, aids identification, and planning of individualised strategies to facilitate diabetes self-management.
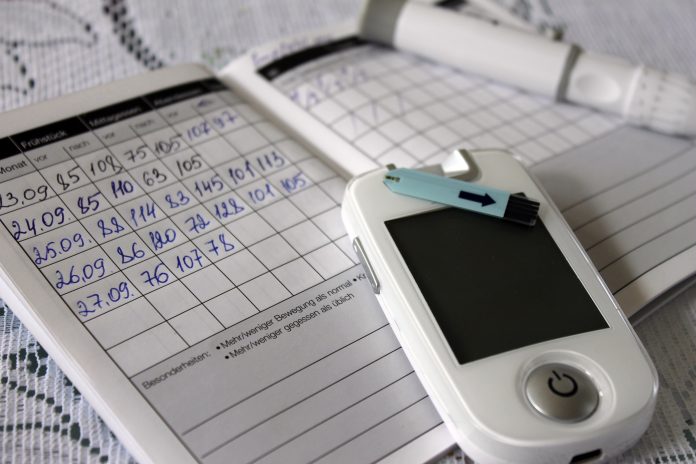
Person-centred and discussion-oriented courses can focus on what the participants want to get out of the programme, while building upon attendees’ experiences. Participants should set themselves goals, and clinical and biometric data should be captured at six and twelve-month time points in order to analyse progress.
Meeting the needs of the diverse & remote population
Due to the impact of COVID-19, many healthcare providers were unable to operate face-to-face consultations during the peak of the pandemic. It also changed the need for people to leave their homes, accelerating the need for digital transformation across the industry.
Agility and flexibility have been fundamental to the continuity of healthcare, and therefore, structured diabetes education providers must adapt to this change and offer an alternative virtual model. By using video conferencing and chat facilities to provide specialist education, this can help to engage patients and encourage dialogue, which is an important part of these programmes – while keeping access to education running wherever the individual may be, or on a digital self-learning basis.
Digital self-learning SDE enables the user to gain access and learn about their condition in their own time, wherever suits them, and at their own pace. This enables the learning to be based around the person’s needs and lifestyle. By having these various options available, SDE courses can remain flexible – which will help to keep the person motivated to attend as and when suits them.
It is also fundamental that SDE courses are made available in a range of languages to suit the patient population and expand upon programme accessibility. Having access to education for patients who are newly diagnosed with diabetes from all ethnicities is crucial, as many will be anxious about their condition and must be supported. Healthcare providers should ensure that their SDE courses are universal in order to meet more patients’ needs, particularly for those people who may not have English as their primary language.
Beneficial outcomes of understanding diabetes
By having SDE programmes in place, with a specific focus on goal setting and a change of diet, the benefits for both patients and the NHS are significant. In terms of lifestyle, by having a diabetes educator available to assist and educate patients, they will become more confident and gain a better understanding of their condition.
This permanent change in mindset empowers patients to take control, and by having the insight into foods with lower glycaemic indices and portion control, as well as the benefits of regular exercise, it can lead to improved clinical outcomes such as weight loss, a reduction in HbA1c and improved glycaemic control.
Consequently, patients having more confidence and improving their overall health and lifestyle choices has a knock-on effect on also benefiting the NHS – both in terms of costs and resources. By reducing the number of diabetes complications, as well as the medicines used, cost savings can be achieved across the healthcare industry. Additionally, increasing the provision and uptake of diabetes self-management and education courses can also reduce risk factors and minimise the chance of developing further health complications, ultimately reducing NHS resources due to needing fewer care interventions, as well as costs.
Building confidence and self-management of diabetes
By putting the patient in control of their condition and helping them to achieve a better understanding of type 2 diabetes through SDE courses, they can build their confidence and self-management of their condition to make positive lifestyle changes and live happier, healthier lives.
It’s important to make more people aware of the help and support that is available, both physically and virtually, while ensuring that SDE courses are designed to increase uptake and help patients gain a better understanding – while empowering them to take control of their condition.