David Bloomfield, Consultant in Clinical Oncology Sussex Cancer Centre, argues that precision radiotherapy is our most effective cancer treatment and should be available to everyone with cancer, but workforce planning is failing our patients
Radiotherapy is a highly effective cancer treatment. This is because it consists of high-energy X-rays that damage cancer DNA such that the affected cancer cells cannot replicate, and instead, they die. As cancer cells grow faster than normal cells, radiotherapy has a disproportionate effect on them.
Radiotherapy’s effectiveness and safety have been recognised for well over a hundred years and have become increasingly sophisticated thanks to developments in technology and computing power. The application of technological advances means we can target specific cancerous areas, sparing healthy tissue. This combination of effective cancer cell killing and targeting makes radiotherapy a potent anti-cancer treatment.
Radiotherapy for cancer treatment
Let’s look at an example: breast cancer is a complicated illness. It is initially a local disease, originating in the breast, but capable of spreading to other tissues and organs. The main use and advantage of radiotherapy in breast cancer treatment is when it is applied to the initial cancer site in ways that both prevent spread and enable safe breast-conserving oncoplastic surgery. Until as recently as 30 years ago, even pea-sized lumps were treated with a mastectomy. It was believed that this extensive surgery offered a better outcome, and it took years of clinical trials to prove conclusively that for most women, this was not the case.
With modern radiotherapy treatment, if the breast cancer is removed with a margin of normal tissue around it (to provide a healthy distance between the tumour and the surgical cut), and the rest of the breast tissue is healthy, radiotherapy will sterilise the cancerous area while keeping the breast intact; this is as safe and effective as having a mastectomy. We also now know that fewer fractions of external beam radiotherapy for early breast cancer are safe and effective and can now be the standard of care. In addition, the cosmetic outcome of radiotherapy for breast cancer is better than mastectomy. As a consequence, the majority of breast cancer patients can safely carry on life without a mutilating operation, which is infinitely preferable for body image and mental health.
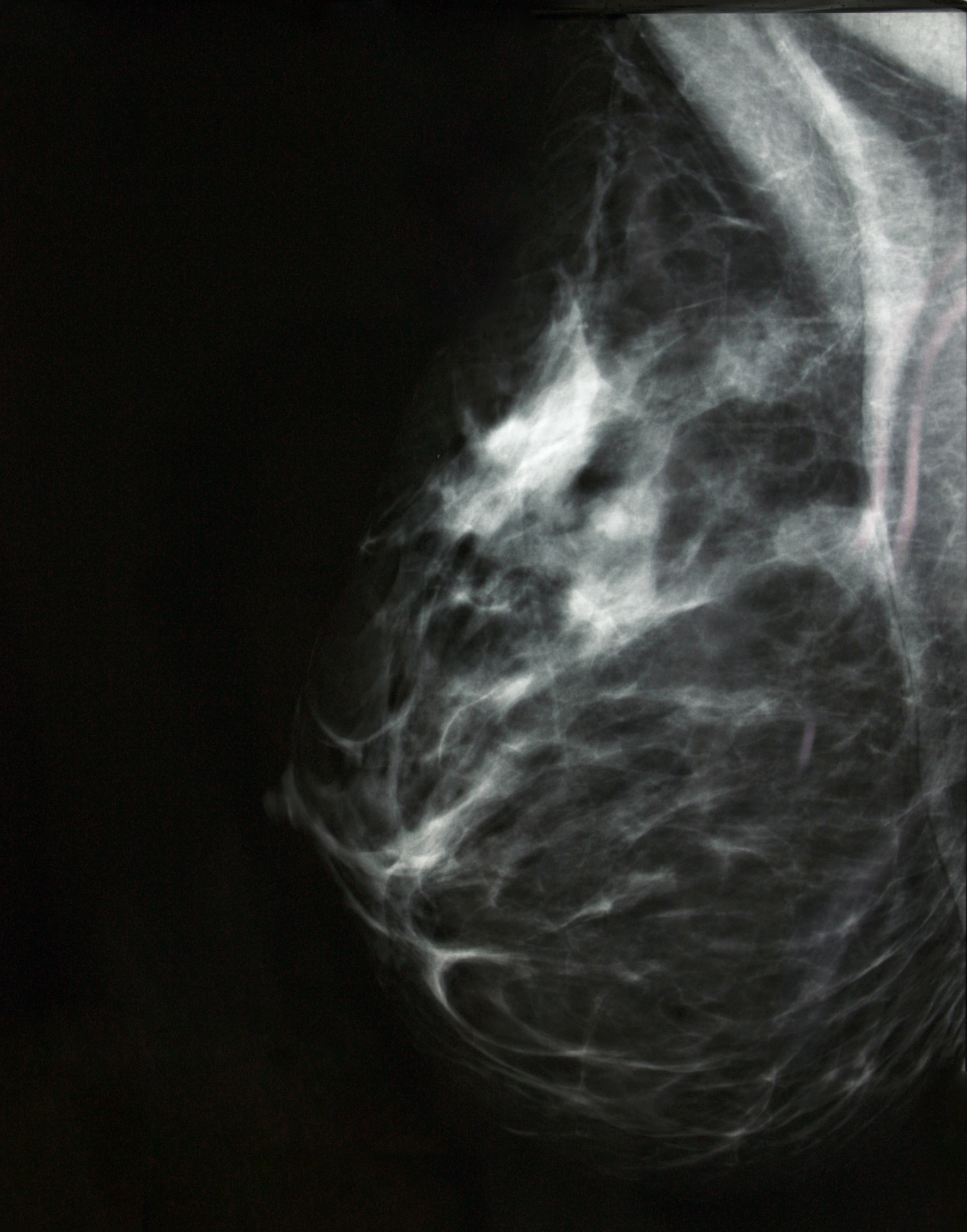
Not only is radiotherapy enormously effective for the safe conservation of the breast itself, but there is also mounting clinical evidence that extending the radiotherapy treatment to areas such as draining lymph glands can improve curative outcomes. Technological developments in radiotherapy now allow accurate targeting of lymph glands under the breastbone, in the armpit, and above the collarbone. This ability to safely treat areas we could not access previously increases the effectiveness of radiotherapy.
It is now internationally recognised that at least half of patients with any type of cancer should have some radiotherapy in their treatment journey. It plays a major part in the cure of many cancers and is an important adjunct in palliative treatments aiming to control those incurable cancers. Yet the proportion of the entire NHS cancer budget allocated to radiotherapy is just 5%. Radiotherapy is incredibly cost-effective, but capital resource intensive. New cancer drugs can cost around £3k a month to administer, adding an average of two months to overall survival, but do not require as much infrastructure and expertise as radiotherapy, and can often start immediately.
Invest more in radiotherapy
It takes significant budgetary planning and commitment to set up a cancer centre with radiotherapy machines, but to not do so is short-sighted. Once up and running, patient numbers coupled with efficient administration (leading to a high throughput), make a radiotherapy department incredibly cost-effective.
If the NHS cancer budget allocation to radiotherapy were increased from 5% to 7.5%, radiotherapy in the UK would be transformed from being a good social medicine service to being world-class. This constant budgetary pressure has had a knock-on effect on resources, particularly radiotherapy staff: we do not have nearly enough people accessing training opportunities to join the profession, nor are we managing to retain them in the profession.
The Radiographers – who run the radiotherapy service – need exceptional knowledge (degree level applied science), emotional skills, communication skills, information technology skills, and team working skills. People with this skillset are at a premium and could fit the criteria for any job, in any industry. For them to engage in a career in radiotherapy (which undoubtedly is a rewarding one) and stay despite the huge pressures of an underfunded, under-resourced health service, is a big ask.
The UK government needs to invest much more in this safe, effective, cost-efficient cancer treatment, and commit to the future of precision radiotherapy. The prolonged neglect of radiotherapy has led to catastrophic workforce shortages (therapeutic radiographers, medical clinical oncologists and physicists) such that staffing is now the major limiting factor for cancer patients getting radiotherapy. We are failing our cancer patients.