Parkinson’s Disease affects all activities of patient daily living but Personal Kinetigraph (PKG) can help
Parkinson’s Disease is caused by the neurodegeneration of dopaminergic neurons, mainly in the basal ganglia. Parkinson’s patients develop motor and non-motor features. As patients start on the treatment primarily for symptomatic control, their motor symptoms can fluctuate depending on the absorption and half-life of the medicine. They can have good control of symptoms which can be misleading for the clinician during assessment in the clinic as they may have pre-dose wearing off and even post-dose dyskinesia. As fluctuation in symptoms affects their activities of daily living, PKG helps to identify these fluctuations (pre-dose wearing off, post-dose dyskinesia, poor symptoms control, compliance to the medications, delayed on of symptoms, tremors, hypersomnolence, ICDs and non-responders requiring review of the diagnosis).
Below are several examples of where the PKG has been used to support the management of the patient’s symptoms and aid in clinical decision-making.
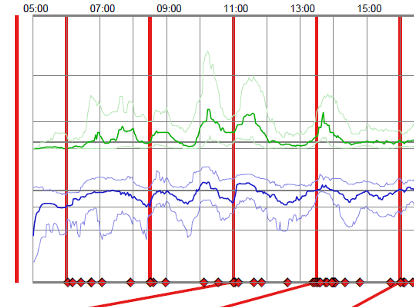
Pre-dose wearing off
This patient attended my clinic for follow-up. Her symptoms were so well controlled that no one could tell she had Parkinson’s Disease. Her PKG showed severe pre-dose wearing off, as above (next column).
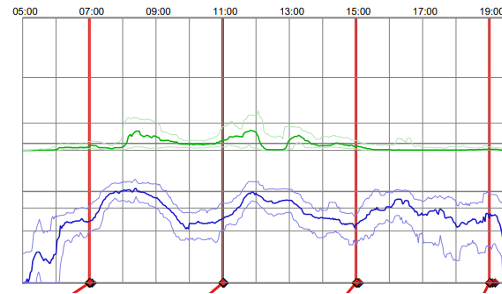
The options for this patient were either increasing the frequency of the Levo Dopa-based medication or adding enzyme inhibitors to reduce wearing off. We opted for both options.
While this patient with pre-dose wearing off only required adjustment in the timing of his medication.
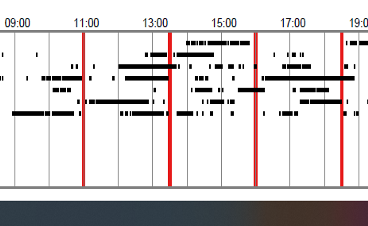
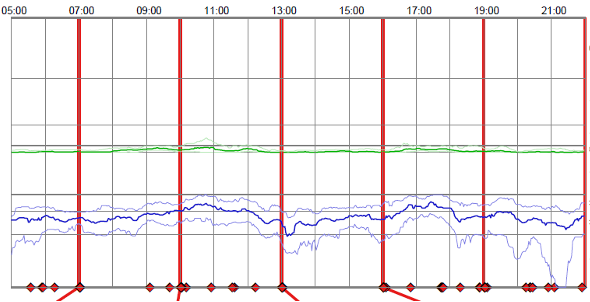
Pre-dose wearing off with post-dose Dyskinesia
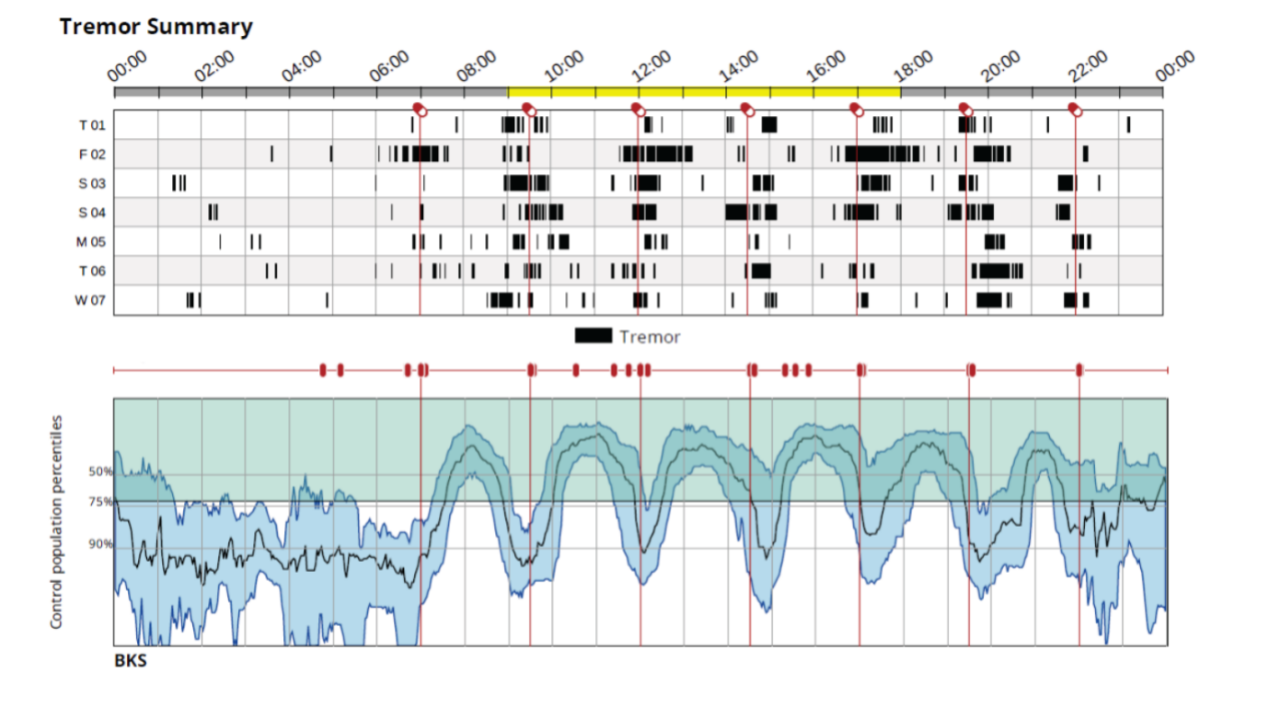
This is a very complex issue when a patient has both pre-dose wearing off and post-dose dyskinesia, as happening in one of my patients as above (next column).
He is having pre-dose wearing off and taking his medication every 2.5 hours throughout the day and every 3 hours through the night. He has severe pre- dose tremors and then post-dose dyskinesia. He was started on Apomorphine, but one day he felt so unwell that he injected the whole of his day’s Apomorphine dose in the first hour by repeatedly boosting himself. He had assessments for Duodopa and DBS and was deemed unfit. He is currently on maximum oral therapy.
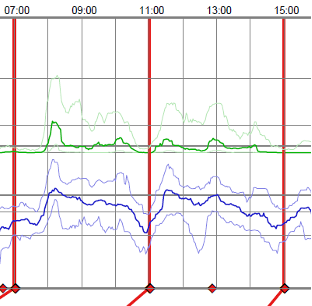
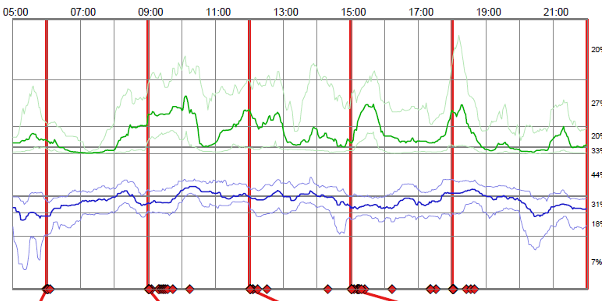
Delayed On
Sometimes patients feel the tablet is not working or taking too long to work, as depicted above (see next page).
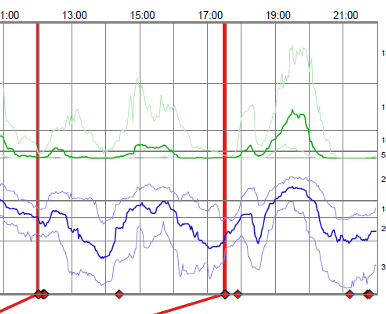
As we can see this patient was taking up 3 and even 4 hours to peak and we found out that he was constipated, which he felt “normal” for him as his routine was one or twice bowel opening per week. Adding laxatives improved his Parkinson’s control.
Non-Responders to L-Dopa
This patient was referred to me as he was not responding to his Levo-Dopa as below.
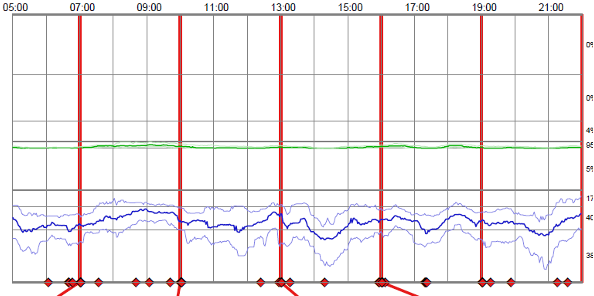
PKG showed no response to Levo Dopa, so the dose was increased and a repeat PKG performed.
There was still no response to high doses of Levo Dopa, so his diagnosis was changed to vascular Parkinsonism.
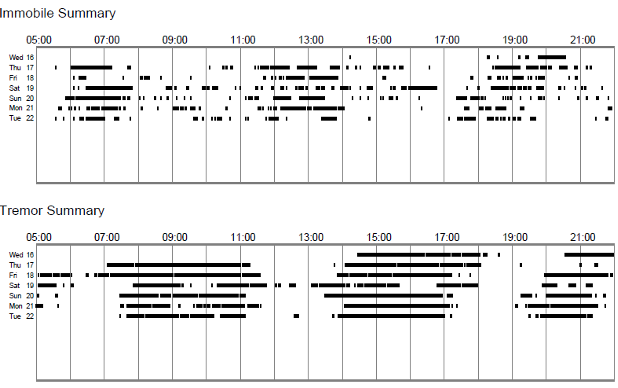
Alternative diagnosis
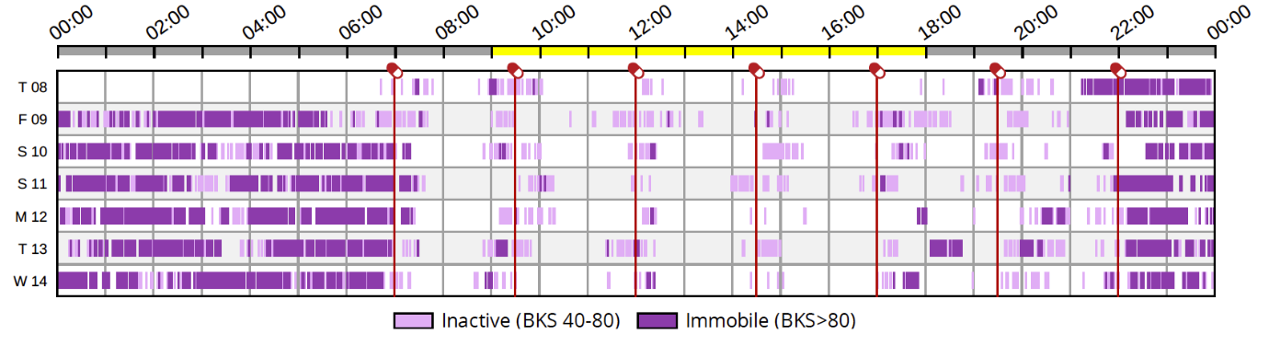
This patient, who was referred as having severe tremors Parkinson’s Disease, had his PKS as above.
PKG showed that the patient had severe tremors only when active and no tremors when immobile, so a diagnosis of Essential tremors was made.
Referral for advanced therapy
This patient was referred to me with wearing off and poorly controlled symptoms and for consideration of Apomorphine. Her PKG is above (next column).
PKG did not show the wearing off and minor adjustments in her oral medications avoided going on Apomorphine infusion.
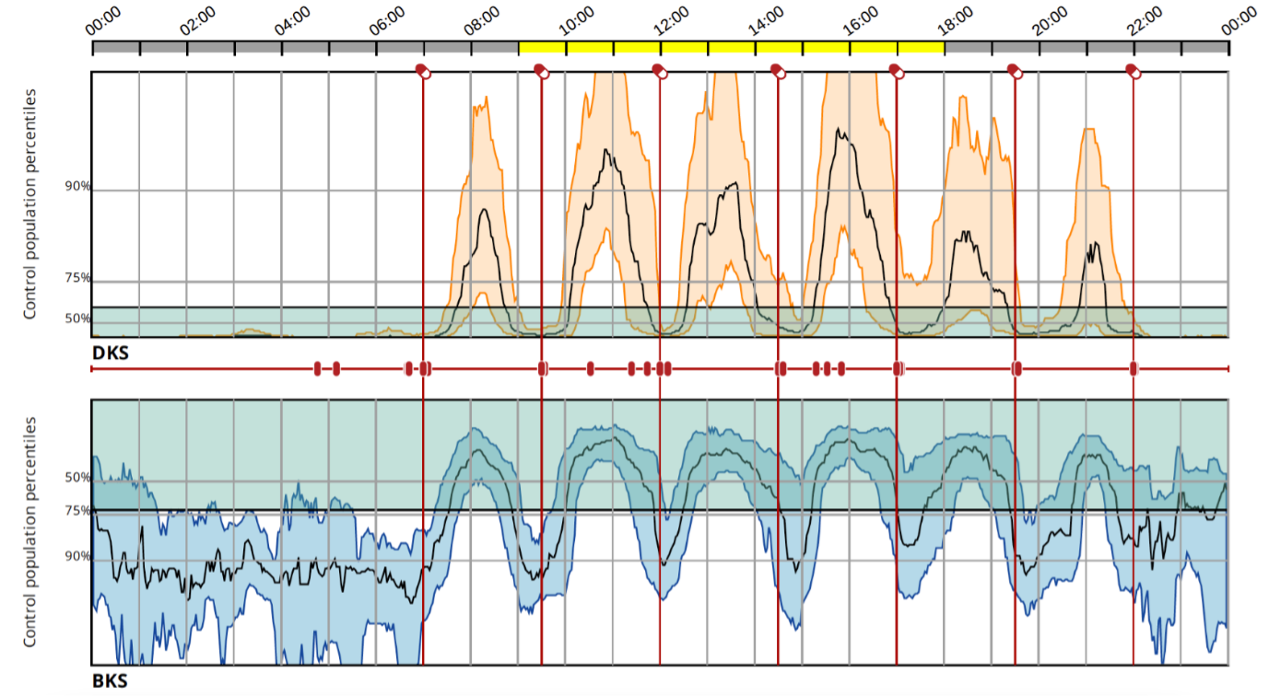
24 hours PKG helps identify night-time symptoms control
Now we have 24 hours PKG which will help to identify night-time symptoms control and will be good for assessing patient sleep pattern, REM sleep behaviour and mobility.
Parkinson’s Disease affects all activities of the patient daily living, but PKG can help
Parkinson’s Disease affects all activities of patients daily living, and PKG can help to identify the control of their symptoms. It helps to identify pre-dose wearing off, post-dose dyskinesia, delayed on, tremors, daytime somnolence, compliance to the medications and adjustment in timing, frequency or dose of the medicines can help to improve patient symptoms. It helps to identify an alternative diagnosis. It helps to identify patients for advanced therapy. It is a cost-effective way of managing patients by reducing appointments, hospital admissions and identifying appropriate patients for the advance therapy. It helps improve patient quality of life, reassure patients about their symptom control, and improve patient satisfaction. It helps monitor patients remotely, which is cost-effective and improves patients’ symptom control.


This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.