Better blood transfusion outcomes for patients and better protection of the NHS blood supply can be achieved with machine learning, argue Drs Samuel McDermott, Nicholas Gleadall and Sara Trompeter
The availability of blood for blood transfusion support is critical for the delivery of medical care. When a person donates blood, it is separated into different components: red cells, platelets, white cells and plasma.
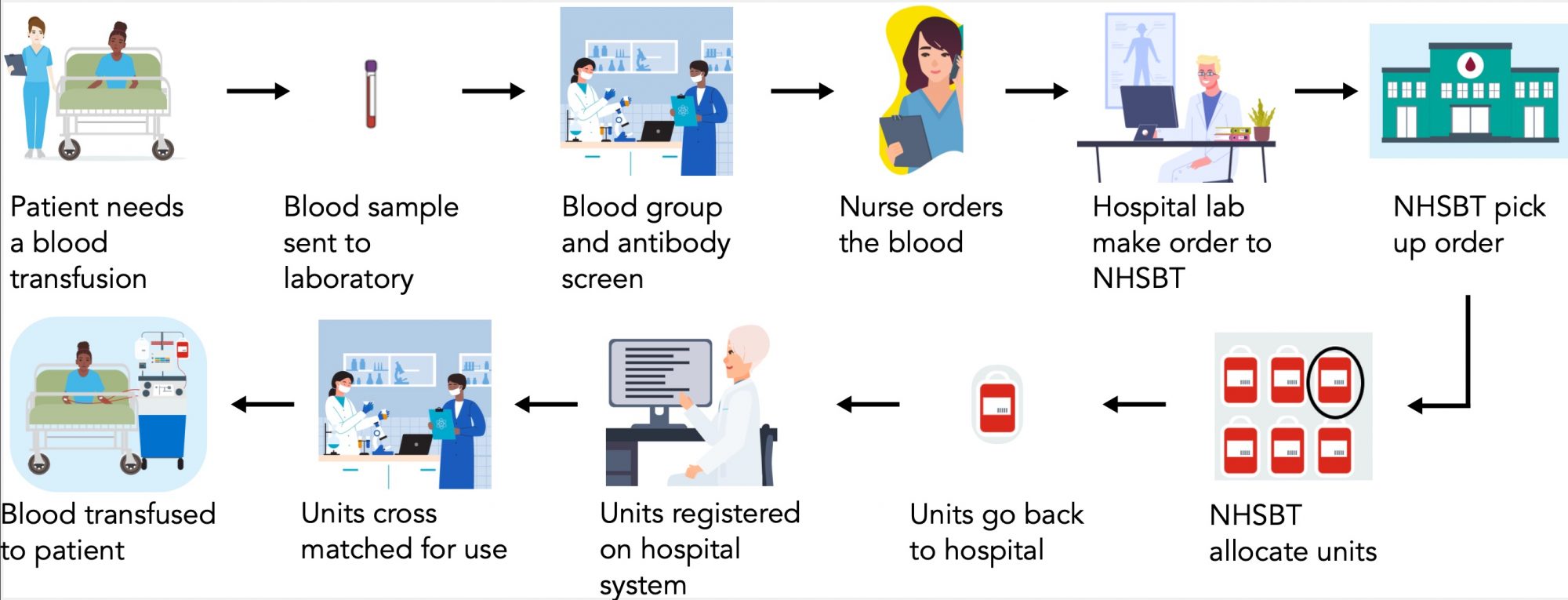
Red cell transfusion is used to treat patients who have lost red cells due to trauma or surgery or who are unable to make healthy red cells. To support over 500,000 transfusions annually, NHSBT issues 1.4 million blood units collected from 800,000 donors.
Blood groups must be matched for transfusion safety
Red cells have ‘labels’ or antigens on their surface, which the immune system can recognise. It is a person’s unique combination of red cell antigens which make up their blood group. Most people have heard of the A, B and O antigens of the ABO system however, there are over 300 other blood group antigens which are important to match for in transfusion-dependent patients.
If a patient is transfused with blood containing an antigen ‘foreign’ to them, they may form an antibody against it. If the sensitised patient is subsequently transfused with the same antigen mismatch, their immune system may destroy the donor red cells in what is called a haemolytic transfusion reaction (HTR). HTRs can make patients extremely unwell and can even be lethal.
Currently, the NHS matches blood for compatibility with the ABO group and RhD (the ‘+’ or ‘-’) antigen in all patients and a slightly extended set of antigens (C/c, E/e, and K) in transfusion-dependent patients. Sensitisation to other medically significant blood group antigens is ignored under current practice, and matching is only carried out ‘reactively’ once antibodies have been formed. This policy leads to direct patient harm that is avoidable if matching practices are improved.
Some patients depend on regular blood transfusions
In the UK, several thousand people depend on red cell transfusion – e.g., those with anaemia or blood cancer. Individuals with inherited blood cell production diseases, such as sickle cell disorder (SCD) or thalassemia, often require transfusions every two weeks for extended periods and, in some cases, for their entire lifetime. Each month over 10,000 red cell units are used to treat people with SCD in England.
People who are regularly transfused are at the greatest risk
A recent audit in the UK showed that 17% of patients with SCD or thalassaemia have red cell antibodies. Further complicating blood matching for sickle cell patients are the differences in blood type frequencies between ancestries. Individuals with SCD are predominantly of African ancestry, while 97% of the UK donor population are of European ancestry. This means that blood types common in these patients (e.g., Duffy antigen negativity) are present in <1% of the UK donor base.
The presence of antibodies in combination with rare blood types frequently means that appropriate blood cannot be found, causing delays in blood transfusion support and further sensitisation to blood group antigens. In some cases, no blood can be found, and patients have died as a result.
How can we improve blood-matching practices for these patients?
There are two main barriers which prevent NHSBT from implementing a policy of extended blood matching.
Firstly, current antibody-based methods for extended blood group antigen typing are costly and extremely time intensive. This means that NHSBT can only type 15% of its donors for all medically relevant antigens.
Secondly, the selection of matched blood for patients with complex requirements (rare blood group and multiple antibodies) is currently performed manually by a team of over 1000 specialist scientists.
Blood group genotyping is a new technology for obtaining complete blood groups
An alternative method to antibody-based typing of blood group antigens is to infer blood groups from the DNA sequence of an individual. NHSBT is a founding member of the Blood Transfusion Genomics Consortium – an international collaboration between global blood supply organisations, leading academic institutions, and industry leaders. The consortium has developed a simple-to-use, affordable, high-throughput DNA microarray-based test for typing donors and patients for all relevant red cell, platelet, and white cell antigens. As part of an ongoing global clinical accreditation study, the test has already been implemented in the clinical laboratories of NHSBT and several other blood services around the world. This new development will allow blood services to obtain complete blood group profiles for a large proportion of their donors and allow hospitals to obtain profiles for heavily transfused patients.
A decision support algorithm for blood matching will focus on minimising the risk of antibody formation
For patients to see benefits from genotyping, there must be a decision-support algorithm for extended blood matching.
The UK-based Haem-Match study aims to use artificial intelligence to develop such an algorithm and will integrate it into the routine blood supply chain.
By considering both patient and donor data the algorithm will:
- Improve patient care by providing the best match wherever possible
- Help to manage and conserve blood stocks by optimising blood allocation and limiting waste.
Data from the algorithm will also indicate which patients are most difficult to provide blood for, which will help guide donor recruitment.
This combination of technologies will improve blood transfusions
The BGC and Heam-Match consortia will demonstrate improvements to patient care through the introduction of genomics and AI into routine care pathways. The implementation of blood group genotyping and AI-based precision matching into NHSBT systems will enable a policy of extended blood matching for patients who need it. This will prevent antibody formation and improve the efficiency of care delivery within the NHS.
This research project is a collaborative effort between NHS Blood and Transplant, the Blood transfusion Genomics Consortium, the Heam- Match consortium, the National Institute for Health and Care Research (NIHR), the NIHR BioResource, the NIHR Health Informatics Collaborative, the University of Cambridge, University College London Hospitals, and the University of Oxford. Samuel McDermott, Nick Gleadall, Sara Trompeter.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


