Can the implementation of digital medication audits improve data transparency and accessibility while reducing medication incidents and improving outcomes?
In healthcare, the term ‘digital transformation’ is often linked to huge projects requiring significant investment and taking years to implement. But what about small changes or less ‘exciting’ projects? Can they still have a significant impact for the organisations that implement them, and benefit their teams?
We have been working with healthcare partners for more than 20 years on service and process improvement in a wide range of organisations. Some of the work we have been doing has led to a completely new business area, focussed on improving efficiency in medication audits. With improvements in cloud technology and digital connectivity in healthcare spaces, many historic barriers around digital medication audits have been removed. This has uncovered vast possibilities for digitisation and improvement, which we find extremely exciting!
Digital transformation is an increasing priority for the NHS
The recent merger between NHS England and NHS Digital signals a significant step change in the direction of our healthcare system. It raises the profile and importance of digital as a fundamental part of the overall strategy for healthcare improvement in England and the rest of the United Kingdom.
Digital transformation has long been a priority but rarely at the top of the agenda until now. New integrated care systems will work in partnership more than ever to ensure the best services and levels of care can be delivered to patients.
In pharmacy, we see a real divide between digital and non-digital activity, mostly driven by the availability of problem-solving solutions. In recent years there has been a significant increase in hospital pharmacies installing clever robots to pick and sort medications and an increasing number of hospitals implementing electronic prescribing to improve efficiency and reduce errors.
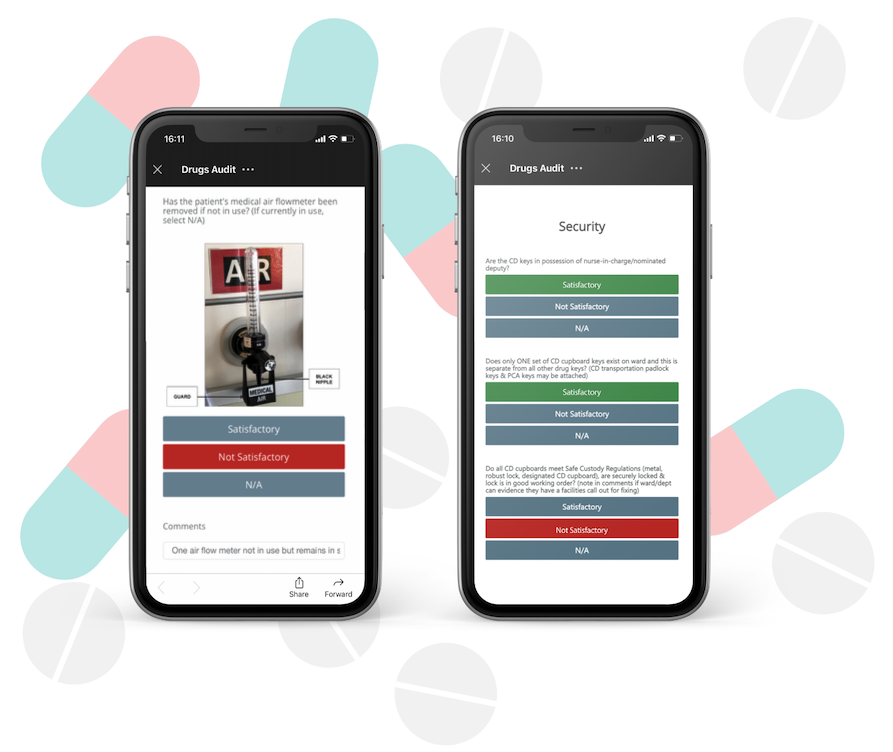
One area that remains on the edge of digitisation is medication auditing. It’s amazing how many places, outside of the expected locations like hospitals and community pharmacies, are having to take responsibility for medication and all the vital administration that comes with it like controlled drugs audits and near-miss tracking.
Marginal Gains: small improvements can make all the difference
When thinking about medication audit processes, the old phrase ‘if it’s not broken, don’t fix it’ might spring to mind. I think we can all agree that this phrase is dangerous in an age of innovation and change. Processes can be seen to be effective and undeserving of change simply because they get the job done. But, in many cases we have seen, a process is continuing because there is no obvious alternative and, more importantly, there is no time or resource to think about change.
Sir Dave Brailsford famously improved the British Cycling team using the concept of marginal gains. The idea that a number of small improvements and changes create a compound effect greater than one single big change took the team from mediocrity to world and Olympic champions! How can this be applied in pharmacy? Does a small improvement that is less time and resource-heavy, allow change to happen incrementally but still have significant impact? We would argue ‘absolutely.’
Small Process, Big Challenge: The potential of digital medication audits
When compared to bigger healthcare challenges, audits may seem like a small task. But the power of any process is in its ability to make something previously painful a pleasure. Imagine having to check back on a written audit document 2 or 3 times to understand it perfectly or having to spend valuable time typing data from paper to PC, not to mention hours of manual data analysis to produce reports. This is the reality for a lot of our pharmacy colleagues, using valuable time on admin that could be streamlined, reducing overall effort and wasted resources, and freeing more colleague time to focus on patient-facing care.
When thinking about how such a small change can make an impact, we urge you to have an open mind. Yes, the audit itself must be done; there has to be a physical check, and someone needs to take ownership of that. But by using a simple, automated solution, any check can be viewed instantly, and corrective measure/s can be implemented quickly, rather than waiting, sometimes several months, for an issue to be noted for action.
Case Studies show dramatic improvement
At Drugs Audit, we are in the process of carrying out time studies and analysing the data to understand the benefits of digital medication audits in terms of resource timesaving. These studies will help us to be clear not only on the potential cost savings to our partner organisations but also on the opportunities for efficiency improvement and enhanced reporting capability.
Early indications from our partners show that the time saving is ‘unbelievable,’ especially when considering the amount of time spent manually analysing data and producing board reporting packs to give confidence in the medication safety process.
The introduction of trend analysis and action planning within the Drugs Audit platform will see organisations take their audits from isolated events to proactive reviews that enable pharmacy teams to actively demonstrate improvements.

Why are digital medication audits so important?
Digital transformation in the NHS and other healthcare organisations is paving the way not only for big eye-catching innovations but also for small improvements in critical areas. By transforming existing medication audit processes, we can support organisations to improve accuracy, transparency and accessibility of audit data, while reducing medication errors and the time and cost burden currently facing our pharmacy colleagues.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.











