This paper describes why the fee system for acute care hospital reform in Japan is beginning to show results
It has been 20 years since the Japanese government introduced a comprehensive fee system (the Diagnosis Procedure Combination/Per-Diem Payment System [DPC/PDPS] ) for acute care hospital reform.
Acute care hospital reform aims to reduce care costs
While the DPC/PDPS was developed to provide visibility into the management and improvement in the management of acute care hospitals, the government’s expected policy outcome was a reduction in inpatient care costs. To date, this goal has not been achieved, partly because the design of the DPC/PDPS is imperfect, and the population is aging, and longevity is increasing. However, other outcomes of introducing the DPC/PDPS are beginning to materialize; the first is an improved quality of medical care through an early discharge and segregation of medical functions, and the other is greater competition in the regional healthcare market.
The medical costs of inpatients are on the rise
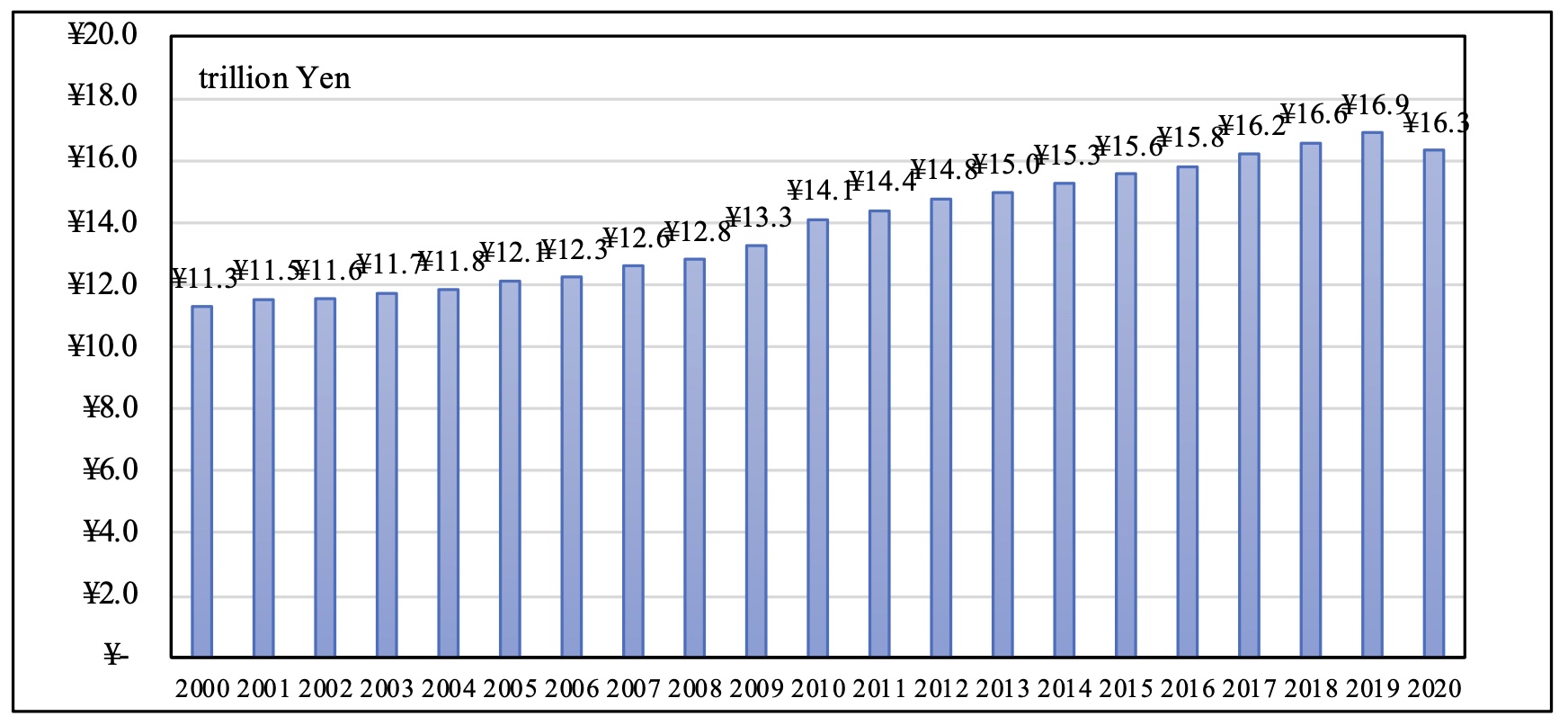
The medical costs for inpatients in Japan have been increasing over the last 20 years, except during the COVID-19 pandemic in 2020. In 2020, the costs reached 16.3 trillion yen, accounting for 38.0% of the national medical expenditure (Figure 1). The reasons include innovations in healthcare technology, population ageing, an increase in longevity, and inefficient provision systems for medical care.
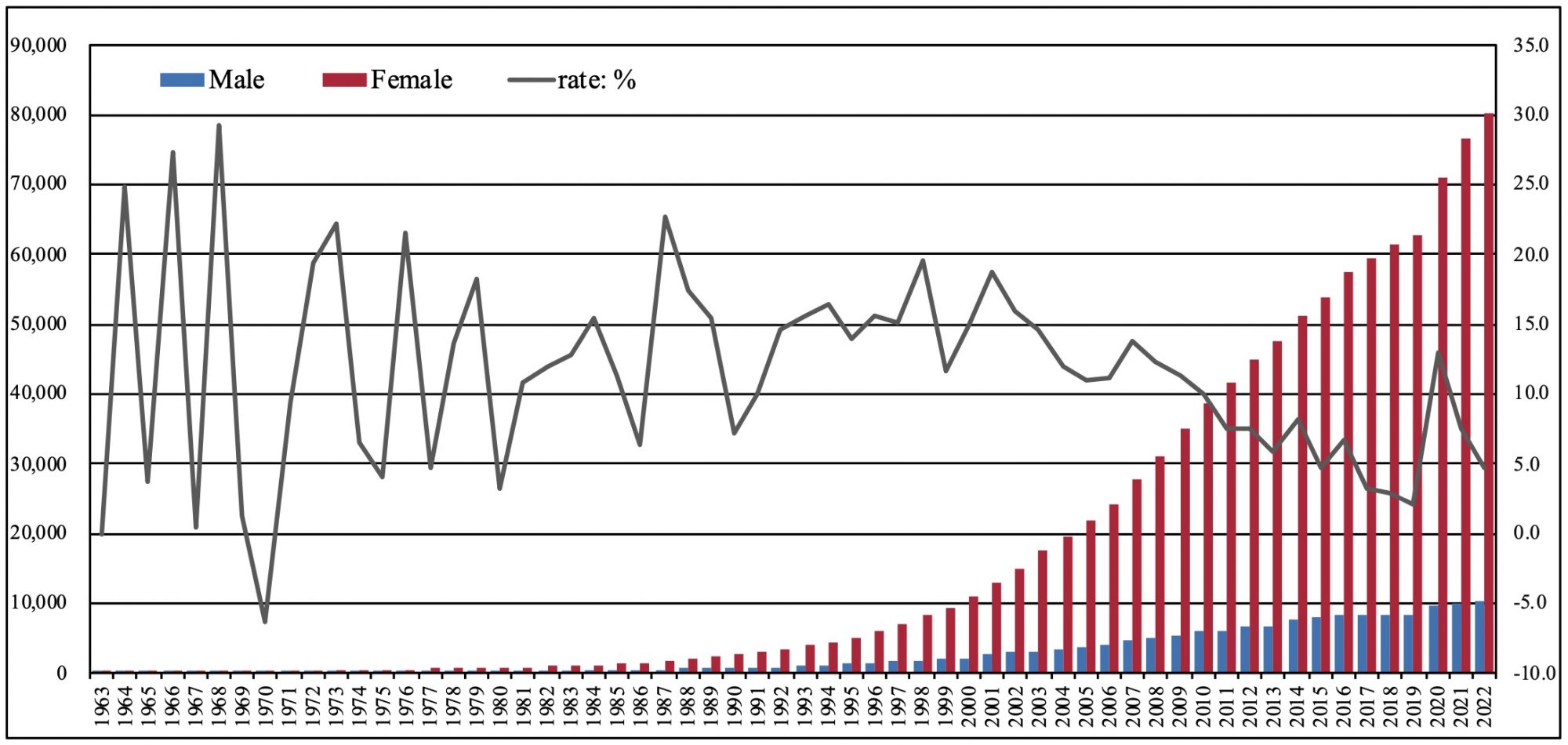
In recent years, newly developed medicines have become expensive, most financed by public health insurance. The ageing rate of the population reached 28.4% in 2019, with 90,526 people aged 100 years and above in 2022 (Figure 2). Many of them require medical and nursing care, which cannot be prevented. In some regions, the need for general hospitals remains high and rural residents value access to smaller general hospitals.
The functional differentiation of healthcare has increased competition in the regional healthcare market
Introduced in 2003, the DPC/PDPS was developed to provide visibility into hospital management and its improvement and provided acute care hospital incentives to discharge patients earlier. Specifically, under this system, the health insurers paid higher fees to acute care hospitals that discharged patients earlier. As a result, many acute care hospitals placed managerial value on discharging patients early and published the early discharge of patients as a surrogate indicator of the quality of care. This incentive could potentially drive hospitals to carry out ‘cream skimming’, as in economics. This implies that some hospitals were likely to refuse to accept patients whose length of stays was likely prolonged.
However, there is no evidence for this phenomenon. The actual phenomenon was the segregation of medical functions within the region. It is a matter of course for hospitals to admit patients to appropriate medical functions. However, this has not been possible in Japan until now, as the rural residents has placed a premium on access to general hospitals, even if they are small.
Furthermore, the segregation of medical functions has gradually increased competition in the regional healthcare market. General hospitals in the region, which traditionally provided all acute, convalescent, and chronic care, lost patients to hospitals specialising in the provision of acute care. The progress in the segregation of medical functions can be largely attributed to the enactment of legislation and increased intervention by the government in line with its policy direction. The fee system for acute care hospital reform has been a major success.
The losers in the regional healthcare market were the smaller public general hospitals
Smaller public general hospitals suffered from increased competition in the regional healthcare market. This paper presents a case study in this regard.
On the Boso Peninsula in south-eastern Chiba Prefecture, east of Tokyo, there are two major hospitals– ‘Kameda General Hospital’ and ‘Asahi General Hospital’ (Figure 3). Both have a long history and have gained dominance in the acute care market, especially in the last 30 years. The hospitals recruited several doctors from abroad who had been providing advanced surgical care and aggressive acute care treatment. Both hospitals’ reputations gradually spread for successful treatment, and they attracted patients not only from within Chiba Prefecture but also from outside the country.
As a consequence, neighbouring public general hospitals suffered financial difficulties and completely lost their market share in the acute care market. Figure 3 shows the location of Kameda General Hospital, Asahi General Hospital and nearby public hospitals. The table on the right shows seven indicators for eight hospitals. Asahi General Hospital (No.1) and Kameda General Hospital (No.5), despite its large bed size and relatively short average length of stay, has a full occupancy rate. The other hospitals (No.2-4, No.6-8) have smaller bed sizes, relatively low bed occupancy and far fewer patients. Asahi General Hospital (No.1) and Kameda General Hospital (No.5) have the largest share of the local acute care market, indicating that they are the patients’ choice.
In 2019, No.2-4 and No.6-8 hospitals were instructed by the Ministry of Health, Labour and Welfare to change their medical functions, that is, withdraw from the acute care market. The result of market competition is to promote the adjustment of healthcare supply and demand through the segregation of healthcare functions in the region. The competition in regional healthcare markets is intensifying throughout the country, which is likely to result in a greater segregation of medical functions.
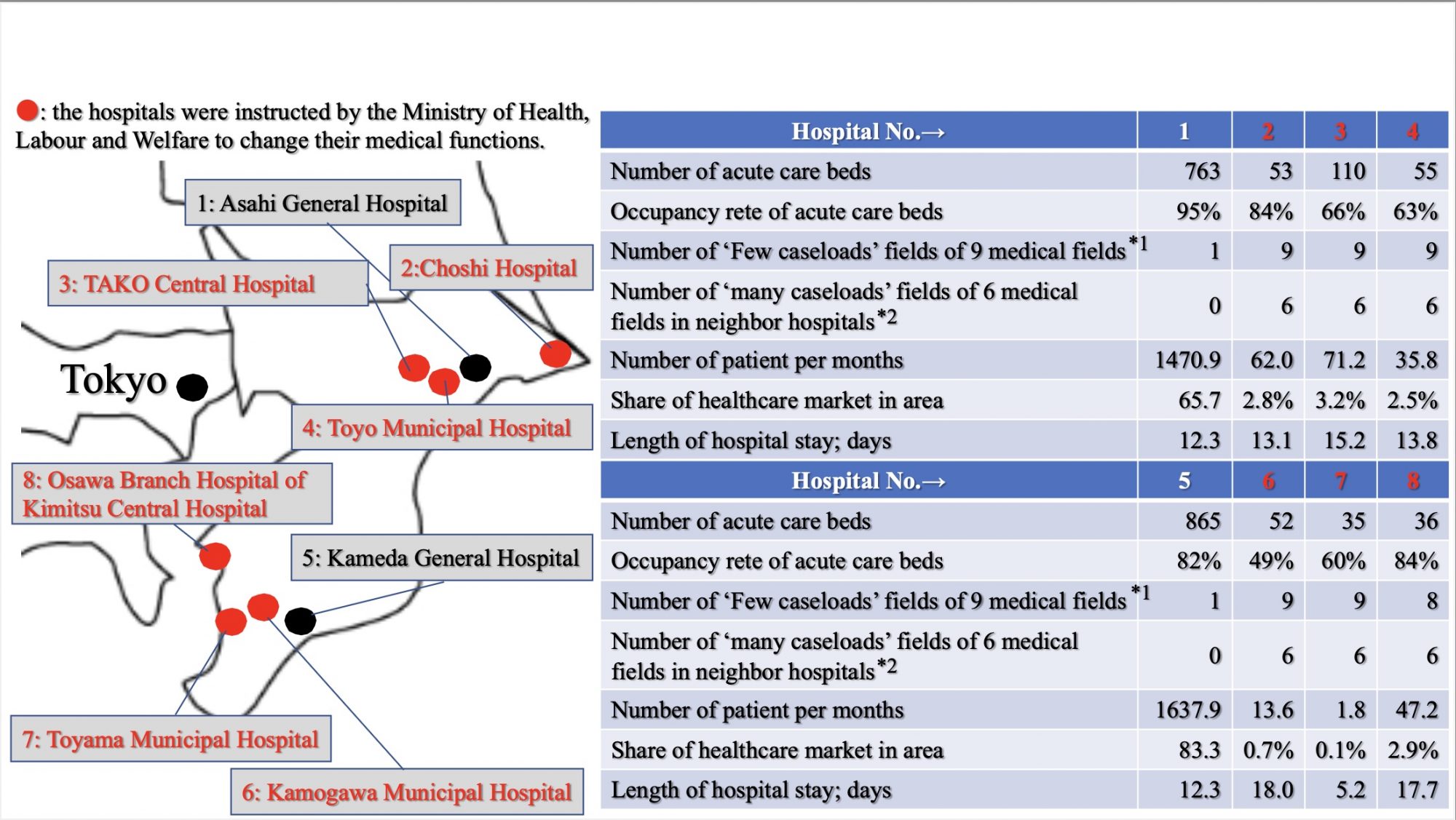
*1: Medical fields are assessed in nine fields; cancer, cardiovascular disease, stroke, emergency, paediatric, perinatal, disaster, remote area and training/dispatch. It is counted as 1 if the number of cases in a medical field is absolutely low. A number of 0 is the highest score and represents a high number of caseloads in nine medical fields. A number of 9 is the worst score and represents a low number of cases in nine medical fields.
*2: Medical fields are assessed in six fields; cancer, cardiac, stroke, emergency, paediatric and perinatal. It is counted as 1, if there is a hospital with a large number of caseloads in the same field in the neighbourhood. A number of 0 is the highest score, indicating that the hospital is so dominant that it has no rivals in the six medical fields. A number of 6 is the worst score, indicating that the hospital is deprived of patients in six medical fields.
Source: Prepared by the author based on documents of “the Working Group on the Vision for Medical Care in the Region, September 2019”.#Drought #Forests #ClimateChange – Climate Service Center Germany (GERICS)
http://bit.ly/3lTT6R6
Importance of segregation of medical functions in the region
Improving the quality of healthcare through the segregation of medical functions is beneficial for both medical professionals and patients. With the segregation of medical functions, medical professionals can expect to accumulate patient caseloads and improve care skills by focusing on patients in specific hospitals. Reciprocally, patients can expect to receive high-quality care in hospitals appropriate for their stage of disease and be discharged early. Greater competition in the regional healthcare market incentivises hospitals to compete with each other for treatment outcomes. It can be expected to result in hospitals that can provide high-quality care appropriate for each stage of the disease. These outcomes of the acute care hospital reform in Japan have not been achieved in time for the arrival of a super-aged society. Nonetheless, they have certainly begun to appear.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


