Bacteriophages have long offered prospects for treating bacterial infections. Is it time to use phages to control tuberculosis? Professor Graham F. Hatfull explores this
Bacteriophages – phages for short – are viruses that infect bacteria. They were discovered about 100 years ago and are prevalent throughout the biosphere and indeed throughout our bodies.
Phages infect and kill bacteria as they replicate, and because of this antibacterial action, they have long been recognized as having therapeutic potential. This potential was largely side-lined once broad-acting antibiotics were discovered, but the troubling emergence of antimicrobial drug resistance has prompted the revisitation of bacteriophage therapeutics.
Phages are different to antibiotics
Bacteriophages differ from antibiotics in several important ways. Firstly, where antibiotics are small, highly active chemicals often with associated toxicities, phages are biological entities with the capacity to replicate and evolve and are not toxic. Phages are larger than typical antibiotics, and this influences how and where they can travel in the body. Unlike antibiotics, phages are potential targets of the immune system, which might limit their applications.
And perhaps most importantly, phages can be very specific for individual bacterial strains, unlike broadly acting antibiotics. But this specificity is a double-edged sword. On the one hand, phages are like guided missiles targeting bad bacteria, leaving good bacteria in our microbiomes unharmed. On the other hand, their specificity confounds the development of generalized treatments, often requiring personalization for individual patients.
Are there phages that infect Mycobacterium tuberculosis?
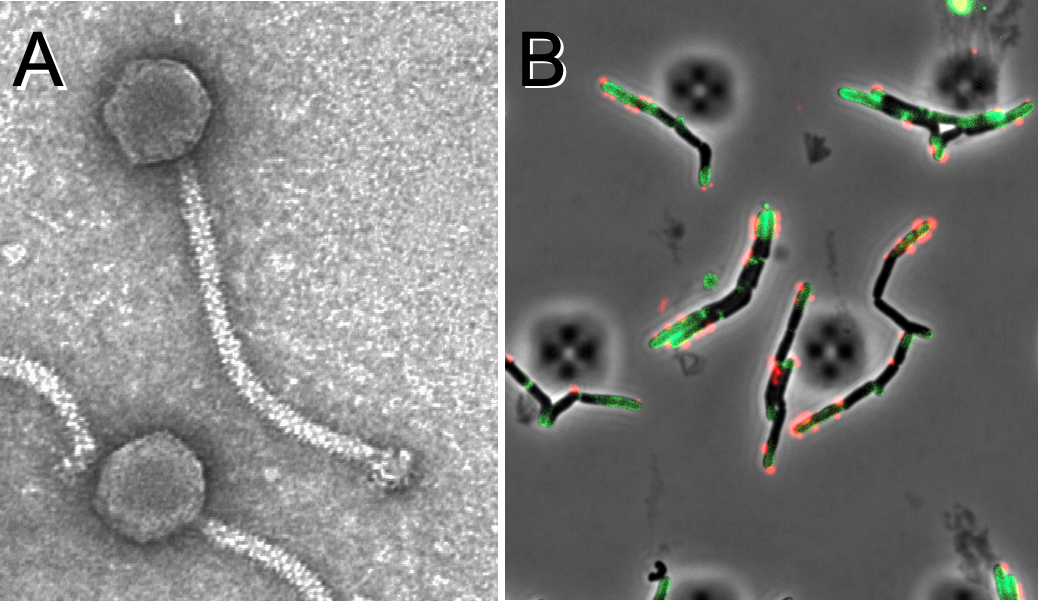
Yes indeed. M. tuberculosis (Mtb) is one of many important species within the genus Mycobacterium, and phages of mycobacteria (i.e. mycobacteriophages) have been described. Mtb is a slow-growing pathogen, so the process of isolating new bacteriophages from the environment using Mtb can be technically challenging. However, the fast-growing non-pathogenic Mycobacterium smegmatis is a superb host for phage isolation, and over 12,000 individual phages have been discovered; 2,200 have completely sequenced genomes (1).
This genomic information provides an important framework for understanding their relationships and their diversity. Moreover, their genomic patterns can be correlated with which ones also infect a laboratory strain of Mtb. Although not all bacteriophages isolated on M. smegmatis also infect Mtb, a few key ones do. And an important and interesting finding is that these phages often infect various clinical isolates of Mtb, reflecting the overall genetic coherence of Mtb(2). Thus, personalization of phage therapies for TB may not be necessary.
What have we learned from using phages to treat nontuberculous mycobacterium infections?
Unfortunately, the clinical use of phages to treat TB has not been explored, and its potential remains unknown (3). However, recently phages have been used on a compassionate use basis to treat several patients with highly antibiotic-refractory nontuberculous mycobacterium (NTM) infections.
These cases shed considerable light on the prospects for phage therapy for TB. First, it must be appreciated that patients eligible for such experimental treatments are very sick, often with multiple challenging conditions, that have run out of options for treating their NTM infections. Second, the good news is that several of these well-documented cases suggest phage interventions can indeed be therapeutically beneficial with favorable clinical or microbiological outcomes.
A consecutive series of 20 cases included five for which no outcome could be determined, but of the remaining 15, 11 showed favorable outcomes, with four having no evident improvement (1). Each of these cases required personalized treatments based on strain screening to identify suitable phages, and phage engineering was required to optimize infection and bacterial killing. Overall, these are encouraging outcomes, notwithstanding the evident challenges.
What are the impediments to using phages to treat tuberculosis?
Unlike antibiotics, bacteriophages have very strong safety profiles and reports of any adverse reactions are extremely rare, although only very small numbers of patients have been treated with any phage for any infection.
Optimal phage dosages are unknown, but the safety profiles suggest that dose escalation studies to determine toxicity may not be essential. The optimal route of administration – intravenous or inhaled – also requires evaluation. Any clinical trial is likely to require regulated manufacturing processes which can be costly, and patient care and follow up is also expensive. However, clinical trial design can vary enormously, and could be anything from a small targeted early bactericidal assay to a full blown multicenter, randomized, and blinded trial. Carefully defining the goals and how phages might play a therapeutic role is a critical first step.
How might phages fit into an anti-tuberculosis therapeutic strategy?
Expectations of the clinical benefits of bacteriophage therapy for TB should be moderate, and there are many potential challenges. Phages may access extracellular bacteria in an advanced infection, but intracellular bacteria or bacteria within granulomas may be hidden to the phage. A stand-alone phage therapy would seem a tall order.
However, it is simpler to envisage benefits from combination phage-antibiotic regimens, where phages may help to shorten treatments, and perhaps minimize the emergence of antibiotic resistance. Similarly, phages might be useful in combination with new (and expensive) antibiotics to help reduce loss of efficacy of the newly developed drugs due to resistance. Because phages have the capacity to replicate on their target bacteria within the human host, one could imagine that a single relatively large phage dose may be administered, simplifying logistics in the developing world. Finally, there is the possibility of using phages prophylactically to minimize transmission among family and workplace colleagues.
In conclusion, many of the pieces needed to evaluate bacteriophages for TB therapy are now falling into place. The time is now to finally put the question to the test: Is there a role for phage therapy in TB control?
References
- Hatfull, G.F. 2022. Mycobacteriophages: From Petri dish to patient. PLoS Pathog 18, e1010602. 10.1371/journal.ppat.1010602.
- Guerrero-Bustamante et al. 2021. Toward a Phage Cocktail for Tuberculosis: Susceptibility and Tuberculocidal Action of Mycobacteriophages against Diverse Mycobacterium tuberculosis Strains. mBio 12. 10.1128/mBio.00973-21.
- Diacon et al. 2022. Mycobacteriophages to Treat Tuberculosis: Dream or Delusion? Respiration 101, 1-15. 10.1159/000519870.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


