Tiago Costa, Assistant Professor at the Department of Microelectronics, Delft University of Technology, discusses opportunities surrounding low-intensity focused ultrasound in the treatment of major depressive disorder in a minimally invasive manner
Major depressive disorder (MDD) is a prevalent and debilitating mental health condition affecting millions worldwide. While various treatment options exist, including medication and psychotherapy, a significant proportion of individuals with MDD do not achieve full remission or experience adverse side effects from existing treatments. Consequently, there is a need for innovative and effective therapeutic approaches to address this complex disorder.
One emerging and promising area of research is the use of low-intensity focused ultrasound (LIFU) to treat major depressive disorder. LIFU is a non-invasive technique that utilises ultrasound waves at lower intensities compared to high-intensity focused ultrasound (HIFU), which is used for the thermal ablation of tissue. By focusing these ultrasound waves on specific brain regions, LIFU has shown potential in modulating neural activity and potentially alleviating depressive symptoms.
The underlying principle behind LIFU therapy is based on the concept of neuromodulation, which involves the selective alteration of neural activity in targeted brain regions. By precisely delivering ultrasound waves to specific areas, LIFU can potentially stimulate or inhibit neural circuits implicated in depression symptoms (Costa et al., 2023). This localised, targeted approach holds promise for personalised and tailored treatment options for individuals with major depressive disorder.
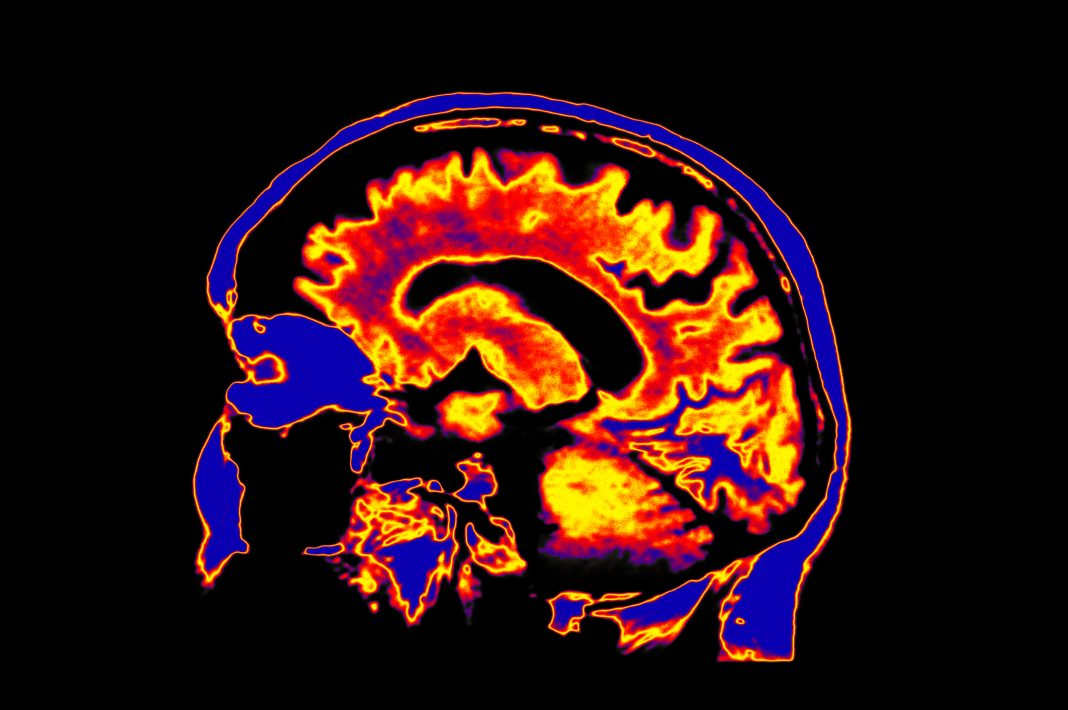
One of the key advantages of LIFU therapy is its non-invasiveness. Unlike invasive procedures like deep brain stimulation, LIFU does not require surgery or the implantation of electrodes. Instead, it relies on the external application of ultrasound waves, which can be precisely guided using advanced imaging techniques, such as magnetic resonance imaging (MRI). This non-invasive nature of LIFU makes it a potentially safer and more acceptable treatment option for individuals who may be reluctant or ineligible for more invasive interventions.
Latest findings in LIFU for major depressive disorder
While LIFU for major depressive disorder is still in the early stages of research and development, preliminary studies have demonstrated promising results. In the first six months of 2023, three new studies have been published where the potential effects of LIFU were demonstrated. F. Wang and colleagues (F. Wang et al., 2023) have shown that LIFU significantly alleviated depression-like behaviours in rats by targeting the medial prefrontal cortex with LIFU after applying the chronic unpredictable stress (CUS) protocol.
Furthermore, these results were achieved with LIFU intensities below the safety limit of 720 mW/cm2 as established in the field of ultrasound diagnostic imaging. These results show promise in the effective and safe application of LIFU for major depressive disorder. Another study (A. Forster et al., 2023) performed a randomised controlled trial by applying LIFU to the right lateral prefrontal cortex with 55 participants and monitoring EEG activity.
By analysing the recorded EEG data, the authors reported that applying LIFU was associated with alterations in the theta activity, correlated with psychological variables such as emotion, cognition, arousal, and other behavioural measures. Finally, in another report (S. M. Guinjoan, 2023), the author hypothesises that LIFU can play a vital role in the pre-surgical selection of optimal stimulation targets for deep brain stimulation. This can potentially improve DBS’s success rate for major depressive disorder, for which only about half of patients show an adequate response.
Ongoing clinical trials exploring LIFU for major depressive disorder
The abovementioned latest results, together with previous years’ findings, have motivated the emergence of several clinical trials for using LIFU for major depressive disorder. These trials typically aim to evaluate the potential of LIFU as a treatment option for individuals with MDD, particularly those who have not responded well to other conventional therapies. In addition to clinical trials, LIFU has been approved as a treatment for MDD in South Korea.
Clinical trials involving LIFU for MDD follow a randomised controlled trial (RCT) design. In an RCT, participants are randomly assigned to different groups, such as an active LIFU treatment group and a control group (placebo or standard treatment). The trials typically assess the effects of LIFU treatment on depressive symptoms, overall mood, quality of life, and functional outcomes. The primary objective of these trials is to determine the safety and efficacy of LIFU for MDD.
They may also aim to identify optimal treatment parameters, such as the intensity, duration, and frequency of ultrasound waves and the targeted brain regions for LIFU application. Additionally, researchers may assess the duration of treatment effects and potential long-term outcomes. Clinical trial outcomes are measured using standardised rating scales for depressive symptoms, such as the Hamilton Depression Rating Scale (HDRS) or the Montgomery-Åsberg Depression Rating Scale (MADRS).
These scales help evaluate the severity of depressive symptoms and assess changes over time. Other measures may include self-report questionnaires, neuroimaging assessments, and functional assessments.
Clinical trials testing major depressive disorder for future treatment
Currently, at least six clinical trials are taking place in North America where focused ultrasound is being investigated for the treatment of MDD, five of which use LIFU rather than HIFU.
At the University of Utah, LIFU is being tested in terms of safety and efficacy across twenty participants while performing psychological and physiological monitoring. At the Laureate Institute for Brain Research, thirty participants have registered to evaluate the effects of LIFU in repetitive negative thinking (RNT), which can be seen as a construct of depression. At the University of Texas, Austin, and the Neurological Associates of West Los Angeles, LIFU is being applied to participants’ amygdala and subgenual cingulate, respectively.
LIFU is applied during several sessions, with psychological and physiological assessments revealing the effects of the trial. Finally, a clinical trial with 50 participants is being conducted at the Ocean State Research Institute, Inc, where the Brainbox BX Pulsar 1002 focused ultrasound transducer is being used to deliver LIFU to the brain of participants, while the primary outcome is measured both via neurological assessment and fMRI.
Recent scientific discoveries and a surge in clinical trials have brought about promising prospects for the use of LIFU as a potential treatment for Major Depressive Disorder (MDD). To make LIFU a viable therapy for MDD patients, it is crucial for physicians, medical researchers, and engineers to collaborate in developing optimal stimulation protocols, selecting the most effective targets, and optimising the LIFU technology. By doing so, LIFU can potentially demonstrate a favourable balance between its benefits and risks, leading to widespread acceptance among patients.
References
- Tiago Costa (2023), “Neuronal networks of depression: Pushing the limits of brain stimulation technology”, Open Access Government April 2023, pp.190-191
- Wang F, Cai Q, Ju R, Wang S, Liu L, Pan M, Sun N, Wang X, Wang L, Yang J, Zheng C, Ming D. Low-intensity focused ultrasound ameliorates depression-like behaviors associated with improving the synaptic plasticity in the vCA1-mPFC pathway. Cereb Cortex. 2023 Apr 11:bhad095
- Forster A, Rodrigues J, Ziebell P, Sanguinetti JL, Allen JJB, Hewig J. Transcranial focused ultrasound modulates the emergence of learned helplessness via midline theta modification. J Affect Disord. 2023 May 15;329:273-284
- Guinjoan SM. Personalized Definition of Surgical Targets in Major Depression and Obsessive-Compulsive Disorder: A Potential Role for Low-Intensity Focused Ultrasound? Pers Med Psychiatry. 2023 Mar-Apr;37-38:100100

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.