Dr Deborah Lee from Dr Fox Pharmacy shares evidence on the link between poor mouth care and dementia risk, and the steps needed to promote better oral hygiene
We all live in fear of dementia, and despite extensive research – sadly, no single cause has been found. But one important factor which has recently come to light is the importance of good oral hygiene.
Could not brushing your teeth be a significant factor in developing Alzheimer’s disease (AD), and if so, what can be done about it?
Dental hygiene and Alzheimer’s disease
Alzheimer’s dementia (AD) has a long preclinical phase of ten to 15 years, but it is only towards the end of this period that there is evidence of cognitive decline.
During this time, amyloid protein – the characteristic pathological finding in AD – slowly accumulates within the brain tissue, and as time passes, neuronal damage begins.
A 2023 publication in Critical Reviews in Microbiology suggested that the bacteria P. gingivalis may be a cause of AD. The bacteria produce enzymes called gingipains which kill nerve cells.
P.gingivalis is also a major cause of periodontitis. In addition, P.gingivalis DNA has been found in the brains of those who have died from AD, as they have large amounts of gingipains.
On its cell surface, P.gingivalis carries outer membrane vesicles (OMVs) that produce proteins and enzymes which damage the host cell and stimulate inflammation. These OMVs can enter the brain as they can cross the blood-brain barrier (BBB).
Once in the brain tissue, they accelerate the production of amyloid and abnormal tau proteins and disrupt iron metabolism, leading to neuronal cell degeneration and death. As a result, iron and ferroptosis (cell death) are now being considered possible causes of AD. These changes occur before the diagnosis of AD. Hence P.gingivalis is thought to be a possible cause – not a consequence – of Alzheimer’s dementia.
The need to care for your mouth and teeth over a lifetime
In a 2021 systematic review and meta-analysis, the authors considered a possible link between tooth loss and dementia. They identified 14 studies, including 34,074 patients, of whom 4,689 had a dementia diagnosis.
Those with the greatest number of missing teeth had a 48% increased risk of cognitive impairment and a 28% increased risk of dementia. For each tooth lost, the risk of cognitive impairment increased by 1.4% and the risk of dementia by 1.1%. In addition, 20 or more missing teeth increased the risk of cognitive impairment by 31%, and losing all teeth increased the risk of dementia by 30%.
There appears to be a close association between tooth loss and dementia, but this observational study does not give any information about causation. Dementia patients have difficulty cleaning their teeth and with mouth care. How can poor oral hygiene lead to dementia?
Why could poor mouth care lead to AD?
Tooth loss is the result of poor oral hygiene. Not brushing the teeth regularly results in bacterial build-up in the mouth, causing inflammation of the gums.
Mouth bacteria cause beta-amyloid and abnormal tau protein deposition
Bacteria are transported via local blood vessels and nerve pathways from the mouth directly to the brain, along with inflammatory cytokines. Salivary treponemes have been identified in the trigeminal nerve ganglia. Chlamydia pneumoniae and B. burgdorferi have been found in the cerebrospinal fluid (CSF) of patients with AD. In addition, glial and other neuronal cells in contact with B. burgdorferi are known to produce beta-amyloid and abnormal tau proteins –significant pathological findings in AD.
Periodontitis causes a dental biofilm
Periodontitis occurs when plaque accumulates between the tooth and the gum, forming a dental biofilm. This adhesive membrane contains over 100 species of bacteria, which are protected by a supportive extracellular matrix.
The biofilm has a restricted oxygen supply and is relatively impermeable to antibiotics. Most are carbohydrate-fermenting bacteria which cause an acidic environment, resulting in demineralisation of the teeth and dental caries (tooth decay). In addition, these mouth bacteria can be transmitted elsewhere in the body, leading to other infections such as endocarditis, pneumonia, and septicaemia (sepsis).
Symptoms of periodontitis include bleeding gums at tooth brushing, halitosis, pocket formation, halitosis and loose or wobbly teeth. As chronic inflammation sets in, an inflammatory exudate develops around the teeth and gums. Persistent low-grade inflammation contributes to the overall level of systemic inflammation.
How to remove dental biofilm
We should all understand how to remove biofilm.
This involves:
Tooth brushing removes around 50% of the biofilm, but it will reform over the next three hours. Use fluoride toothpaste and clean your teeth for two minutes twice a day. This should be before breakfast and before going to bed at night.
Flossing removes biofilm from the interdental spaces between the teeth and under the gums. Use a strip of dental floss which you insert between the teeth and use a rocking motion up and down the sides of the tooth and into the gum line. Interdental brushes remove more plaque than dental floss.
Mouthwash containing chlorhexidine gluconate, essential oils (tea tree oil, thyme, and peppermint) and cetylpyridinium chloride have been shown to reduce biofilm.
A dental hygienist is essential as it is virtually impossible to reach all the areas of biofilm at home by yourself. A visit once every six months is recommended, but some people may need to go more often.
Doctors, mouth care and dentistry
Better collaboration between doctors and dentists would have far-reaching improvements for public health. The UK medical curriculum makes little provision for oral health. Your GP rarely asks you if you floss your teeth.
Doctors do not have the skills or equipment to assess dental issues. The World Health Organization (WHO) has recommended training GPs and others in primary care to manage emergency dental problems. However, in one study of 90 patients who presented at A&E with dental problems over six months, almost none received a dental diagnosis. Instead, all patients were treated symptomatically and advised to see a dentist.
GPs see families with small children daily and are in an ideal position to encourage them to practise good oral health. In the US, Harvard has instigated an Oral Physician Program, which brings oral hygiene, primary care and family medicine together. Indeed this is something we should be adopting in the UK.
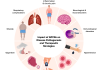
Gum disease can lead to:
- Cardiovascular disease
- Infective endocarditis
- Pneumonia
- Preeclampsia
- Premature deliveries
- Low birth weight babies
- Erectile dysfunction
And now it seems we can add Alzheimer’s Disease to this list.
Preventive mouth care
It is high time to prioritise mouth care. Dementia UK stresses the need for good mouth care for patients diagnosed with dementia. But what about the need to encourage people to care appropriately for their mouths long before a diagnosis of dementia is made? When you look for advice on the internet about reducing the risk of dementia, good oral hygiene and dental care are usually not on the list.
In light of the new evidence discussed above, it would be heartening to see a campaign for better oral health for many health reasons – but including the all-important issue of trying to reduce the risk of AD. Although not proven, chronic mouth inflammation plays a significant role in the pathogenesis of the disease.
Doctors and dentists must take a united and reinvigorated approach towards getting the nation to brush, floss, use mouthwash and visit the dental hygienist.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6354555/#:~:text=It%2
0is%20generally%20accepted%20that,without%20surgical%20intervention%2 0%5B8%5D - https://paperiocenter.com/blog/oral-biofilm-your-home-care/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9219991/
- https://www.sciencedirect.com/science/article/abs/pii/S1525861021004734?via%3Dihub
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312703/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4488989/
- https://www1.racgp.org.au/ajgp/2020/september/medicine-and-dentistry
- https://www.statnews.com/2017/07/17/dentistry-medicine-division/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8041071/