Professor Shaw-Ruey Lyu from the Dalin Tzu-Chi Hospital discusses the benefits of arthroscopic cartilage regeneration facilitating procedure (ACRFP) as an alternative to traditional methods of treating knee OA
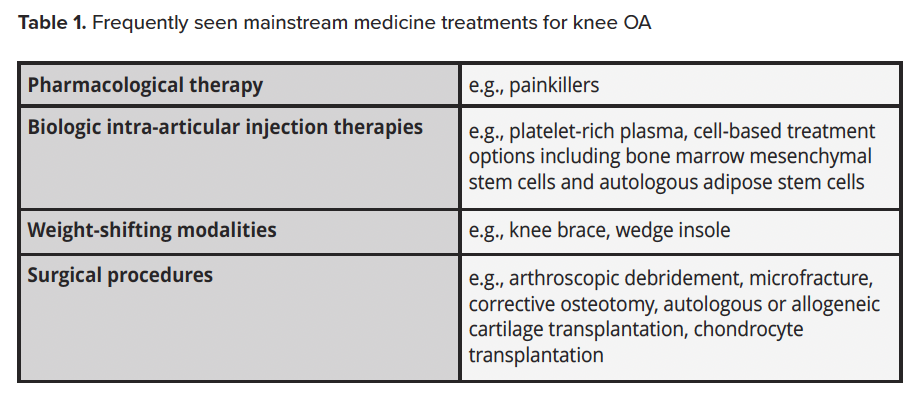
I have always been a conscientious orthopedic surgeon. I was trained in mainstream orthopedic medicine and had treated many patients suffering from knee osteoarthritis (knee OA) with all the available tools in the ‘mainstream medicine’ repertoire (Table 1). Traditional treatment often led patients to eventual knee replacement. That is proof that mainstream medicine cannot stop knee OA from deteriorating, and even lead to patients needing a knee replacement.
So, I looked for a better way. After years of research, I found medial abrasion phenomenon (MAP) to be a neglected but important cause of knee OA, (1) and to treat MAP, I developed a comprehensive treatment protocol – Knee Health Promotion Option (KHPO). (2,3) This offered an improved alternative to the aforementioned mainstream treatments.
KHPO is more effective and less intrusive and has worked well for over ten thousand knee osteoarthritis patients since 2000. After treatment, most patients have been satisfied and can avoid knee replacements.
The arthroscopic cartilage regeneration facilitating procedure (ACRFP) is a key component that has contributed to the success of the KHPO.
What is ACRFP?
The arthroscopic cartilage regeneration facilitating procedure (ACRFP) is an integrated, comprehensive, and novel arthroscopic surgery that aims to remove all existing risk factors of knee OA from the knee, hence eliminating knee pains and making the knee a more hospitable place for the damaged cartilage inside to regenerate. (4,6) The ACRFP eradicates the medial abrasion phenomenon and inflamed synovium and capsule, decompresses the patellofemoral joint, restores soft tissue balance around the patella, removes other known risk factors (synovitis, meniscus tears, and chondral flaps) of knee OA, and, consequently, improves the environment in the knee to be more hospitable to cartilage regeneration. Therefore, knee OA patients who receive ACRFP are much more likely to avoid knee replacement.
How is ACRFP distinct from – and superior to – the mainstream treatment?
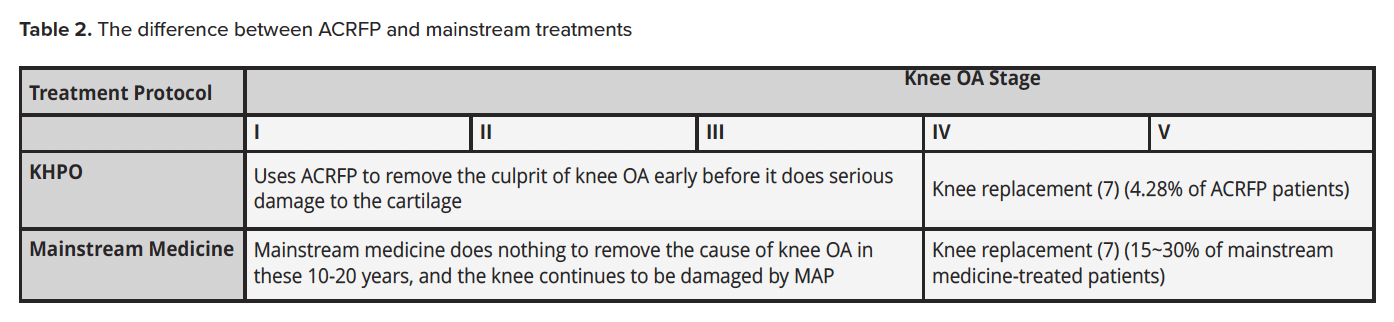
The key difference between ACRFP and mainstream treatments is illustrated in Table 2. KHPO starts using ACRFP as early as possible to treat and remove a cause of knee OA – the medial abrasion phenomenon (MAP) and its sequelae. Mainstream medicine typically does not start major invasive treatment until stage IV, when the knee has deteriorated significantly and requires knee replacement.
The time gap between the early (I, II, III) and late (IV, V) stages could easily be 10 to 20 years. During this time, ACRFP patients are reaping the benefits of having the culprit (MAP and its sequelae) of their knee OA removed, their knee pains relieved, and avoiding knee replacements. On the other hand, during that same period, mainstream medicine physicians did nothing to remove the culprit. Hence, the MAP continues to damage patients’ knees from stage I to stage II, to stage III, and stages IV and V, when knee replacement is almost certainly required.
Early removal of the culprit (MAP and its sequelae) of knee OA is why ACRFP is much better than mainstream medicine in avoiding knee replacement. Traditional therapies fail to target the causes of knee osteoarthritis; much steeper than the monetary cost of patients’ treatment is the price of a missed opportunity to treat knee OA. In other words, if patients take the mainstream treatment, their knees continue to deteriorate, they miss the golden opportunity to eradicate the cause of knee OA, and they risk losing their natural knee to knee replacement.
Conclusion
ACRFP is an active, pre-emptive early treatment to remove the causes of knee OA before the damage becomes irreversible. Unfortunately, mainstream treatment pathways are passive and symptom-relieving without eradicating the causes of knee OA. It imprudently waits after the knee damage is beyond repair and a knee replacement is required. The doctor and, by extension, the treatment protocol, a patient chooses largely determines whether his or her OA knee is saved or replaced.
References
- Lyu SR, Chiang CY, Cherng JY, Huang YC, Li CH, Lin YJ, Chang CM, Chau LK. Role of medial abrasion phenomenon in the pathogenesis of knee osteoarthritis. Med Hypotheses. 2015 Aug;85(2):207-11. doi: 10.1016/j.mehy.2015.04.028. Epub 2015 May 1. PMID: 25957655.
- Shaw-Ruey Lyu (2023), “Knee pain and osteoarthritis (Knee OA) treatment research,” Open Access Government July 2023, pp.48-49. Available at https://www.openaccessgovernment.org/article/knee-pain-osteoarthritis-knee-oa-treatment-research/163045/. (Accessed: 27 Nov 2023)
- Shaw-Ruey Lyu (2023), “Knee health promotion and cell therapy for knee osteoarthritis,” Open Access Government October 2023, pp.170-171. Available at https://www.openaccessgovernment.org/article/knee-health-promotion-and-cell-therapy-for-knee-osteoarthritis/168901/.(Accessed: 27 Nov 2023)
- Lyu SR, Hsu CC, Lin CW. Arthroscopic cartilage regeneration facilitating procedure for osteoarthritic knee. BMC Musculoskelet Disord. 2012 Nov 21;13:226. Doi: 10.1186/1471-2474-13-226. PMID: 23171074; PMCID: PMC3583133.
- Lyu SR. Arthroscopic medial release for medial compartment osteoarthritis of the knee: the result of a single surgeon series with a minimum follow-up of four years. J Bone Joint Surg Br. 2008 Sep;90(9):1186-92. doi: 10.1302/0301-620X.90B9.20584. PMID: 18757958.
- Lyu SR, Hsu CC, Hung JP, Chou LC, Chen YR, Lin CW. Arthroscopic cartilage regeneration facilitating procedure: A decompressing arthroplasty for knee osteoarthritis. Medicine (Baltimore). 2022 Sep 30;101(39):e30895. doi: 10.1097/MD.0000000000030895. PMID: 36181017; PMCID: PMC9524980.
- Lyu SR, Hsu CC, Hung JP, Chou LC. Arthroscopic cartilage regeneration facilitating procedure can modify the clinical course of knee osteoarthritis. J Orthop Surg (Hong Kong). 2023 May-Aug;31(2):10225536231180331. Doi: 10.1177/10225536231180331. PMID: 37395209.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


