Venous catheters enable patients with haematological cancers to receive vital chemotherapy. However, there is a risk of thrombosis. Consultant Haematologist Priya Sriskandarajah analysed a group of patients with haematological cancers to study the implications of catheter selection
Venous catheters in cancer care
Over the years, there have been major developments in cancer care, including novel chemotherapy regimens as well as stem cell transplantation. To support these advancements and enable efficient treatment administration, venous catheters (i.e. ‘lines’) are required. These are surgically inserted into a patient’s vein and allow direct delivery of these treatments into the bloodstream.
Types of venous catheters
There are two main types of catheters – long-term skin tunnelled catheters (LTSTCs) and peripheral catheters (PICC). An LTSTC is surgically tunnelled under the skin into a central vein (usually in the chest) and may remain in place for several months. A PICC is an external catheter connected to a peripheral vein, usually in the arm.
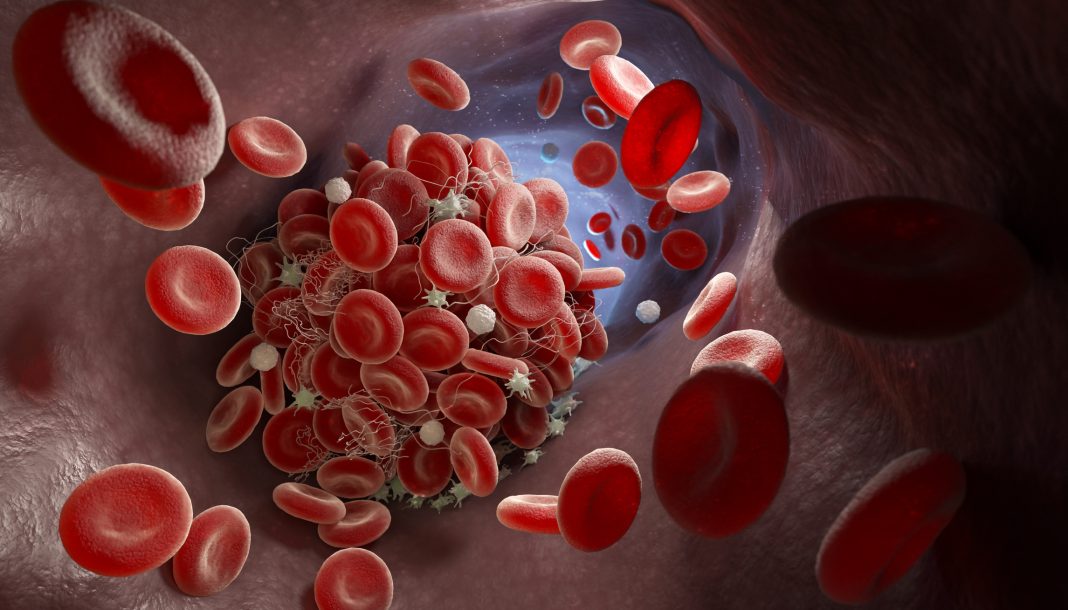
LTSTCs are often used in patients with haematological cancers who require stem cell transplant, while PICCs are frequently used for chemotherapy administration. The advantage of PICCs over LTSTCs is that they are easy to insert and less invasive, thus reducing the risk of complications. However, due to their smaller lumen size, PICCs can cause blood flow to become ‘sluggish’, increasing the risk of clot formation, while this is not observed as much with LTSTCs.
Baseline patient diagnostics
We performed a retrospective analysis of 583 patients with haematological cancers admitted at the Royal Marsden Hospital who had either PICC or LTSTC inserted for treatment administration. 346 patients received a PICC, and 237 received an LTSTC. The haematological cancers included acute myeloid leukaemia (AML), acute lymphoblastic leukaemia, Hodgkin or non-Hodgkin lymphoma, multiple myeloma (MM), and chronic lymphocytic leukaemia.
Increased thrombosis risk with PICC catheters
There was a greater incidence of catheter-related thrombosis with a PICC than with an LTSTC. During follow-up, about one in 20 patients (5.6%) receiving a PICC developed thrombosis versus one in 50 patients (1.7%) receiving an LTSTC. Also, thromboses usually occurred early, within 30 days after insertion, and this was noted in 5% of PICC patients and 1% of LTSTC patients.
The ‘dwell time’ of a catheter line refers to the duration of its placement within a patient’s vein. Typically, LTSTCs are inserted longer than PICCs, which was confirmed in our study. The median dwell time for LTSTCs was almost twice as long as for PICCs (109 days versus 65 days). The risk of thrombosis increased the longer a PICC or LTSTC was inserted. After six months, deep vein thrombosis (DVT) was reported in 14% of patients with a PICC. By comparison, DVT was reported in 6% of patients with an LTSTC after 27 months. Thus, thrombosis risk increased at a slower rate with an LTSTC than with a PICC despite longer dwell times.
Secondary complications of catheter-related thrombosis
Patients with a PICC had more than double the risk of a catheter infection than those with an LTSTC (45% versus 20%). Following a catheter-related thrombosis event, 80% of patients had their PICC removed, compared with 50% of patients who had their LTSTC removed. All patients who developed a catheter-related thrombosis received an anticoagulant medication for three months, and no bleeding-related complications were reported.
Risk factors for catheter-related thrombosis
We also considered the risk factors in patients who developed catheter-related thrombosis. These data were available for 20 patients with a PICC and four with an LTSTC. A previous history of DVT was reported in two patients with a PICC (10%), compared with no patients with an LTSTC. Although there was a small number of patients, this does suggest that DVT history is a contributing factor for PICC-related thromboses. Rates of catheter-related thrombosis were similar between patients with newly diagnosed disease, relapsed or refractory disease, and remission (5.3% versus 6.1% versus 6.5%). These findings suggest that the disease stage does not affect thrombosis risk.
Implications for treatment
The finding of a greater risk of catheter- related thrombosis with PICCs than with LTSTCs, leading to a higher rate of thrombosis-related complications with PICCs, is critical. This is especially important in patients with haematological cancers as this could potentially result in delayed administration of chemotherapy and expose these patients to the risks of anticoagulation (i.e. blood thinners). The latter is particularly important as haematology patients could have prolonged periods of low blood counts induced by chemotherapy, thus increasing the risk of bleeding, although reassuringly, we did not observe this in our study. However, our study findings highlight the importance of assessing the risk of thrombosis in venous catheter selection prior to commencing treatment in patients with haematological cancers. This is particularly true when long-term chemotherapy is needed or when patients have a history of blood clots, as these patients must be continuously monitored.
Future directions
Ours is the largest study to date to specifically examine catheter-related thrombosis in patients with haematological cancers. Given the recent advances in cancer therapy, future randomised control trials comparing PICCs against LTSTCs are required to assess both the short- and long-term outcomes. Importantly, further data is needed to address the debate on whether haematological cancer patients require preventive anticoagulation treatment following venous catheter insertion.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.