As the UK’s healthcare system continues to struggle with care and cancer backlogs, Gareth Jenkins of Changeology Group Ltd explains how the company can assist healthcare teams in making positive operational changes that enhance efficiency and patient outcomes
In the wake of the COVID-19 pandemic, the NHS faced and continues to face unprecedented challenges in cancer care. Unfortunately, 20% of cancer referrals are currently breaching target treatment times, which brings focus to cancer services requiring support. While increased funding is crucial, throwing money at the problem without addressing underlying systemic issues risks perpetuating a cycle of inefficiency and poor patient outcomes.
The roots of the crisis
It’s easy to attribute the current backlog to the pandemic and staff shortages caused by Brexit. However, while significant, these factors were catalysts that exposed and exacerbated long-standing operational inefficiencies within the NHS. The reality is that things were far from perfect even before 2019 or Brexit.
At Changeology, we believe the focus should be on rebuilding the fundamental operating systems within NHS departments. Our experience has shown that many NHS services operate with dysfunctional systems, leading to poor utilisation, reduced productivity, unsatisfactory patient experiences, and diminished staff wellbeing.
The power of effective operating systems
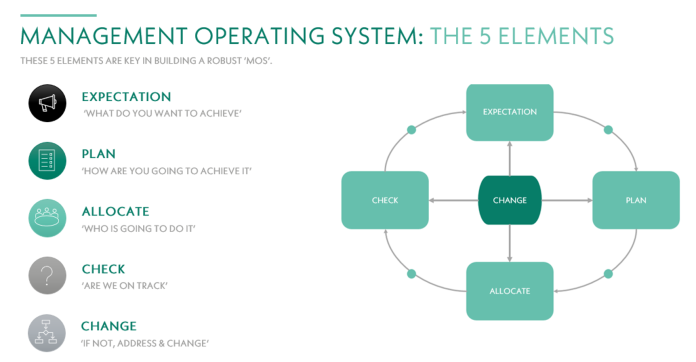
When we talk about ‘systems’, we’re not referring to IT software. Instead, we mean the comprehensive framework that keeps a department or organisation moving—its very lifeblood. A well-designed Management Operating System (MOS) provides the right information, tools, and levers for informed decision-making. It empowers leaders to create growth opportunities, plan effectively and monitor progress to facilitate continuous improvement.
An effective MOS is:
- Performance-focused:
- Driving productivity through the right structure, data, and behaviours.
- Structured:
- Providing clear goals and objectives within a framework for success.
- Data-driven:
- Using facts and metrics to enable meaningful discussions and drive decision-making.
- Geared for continuous improvement:
- Allowing for ongoing enhancement of performance and growth.
- Culture-positive:
- Creating a focused, proactive environment that breeds a better, happier workplace.
Case study: Transforming endoscopy services at UHMB To illustrate the impact of systemic improvements, let’s look at our recent project with the University Hospitals of Morecambe Bay NHS Foundation Trust (UHMB).
Initial situation: UHMB’s endoscopy services were grappling with soaring waiting lists and breaches post-pandemic. The challenge wasn’t just about clearing backlogs but establishing sustainable solutions beyond reactive measures.
Our approach: We conducted an in-depth review of UHMB’s existing systems and collaborated with clinical, operational, administrative, and IT teams to implement comprehensive improvements. Key interventions included:
- Introducing standardised, quantified processes;
- Implementing six-week planning cycles;
- Establishing key performance indicators and reporting mechanisms;
- Providing targeted training; and
- Enhancing tracking and operating systems.
These interventions directly applied MOS principles, establishing a structured, data-driven approach to managing endoscopy services.
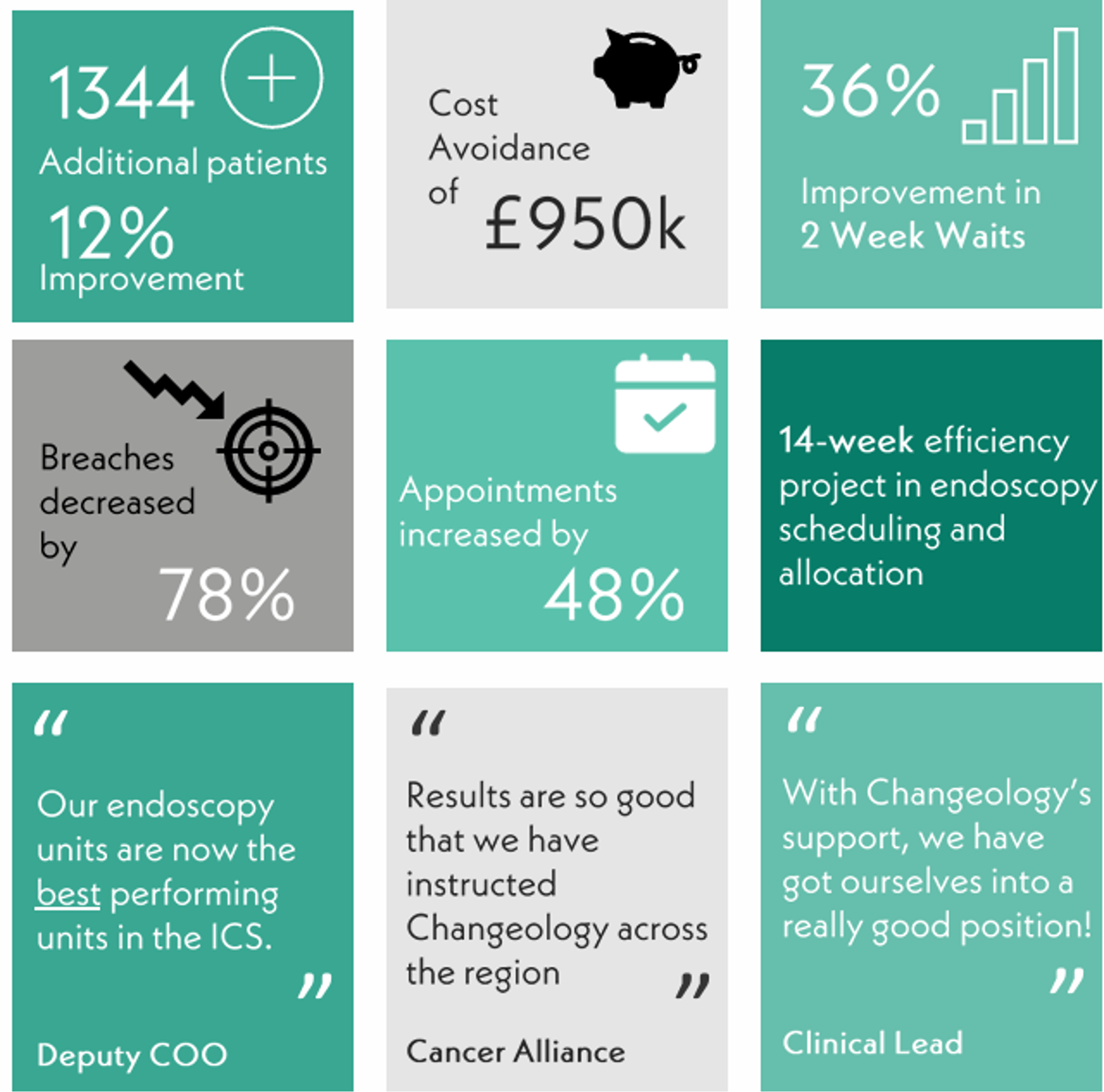
Results: Clearing the cancer backlogs
Beyond the numbers
The qualitative impacts were equally important. Staff reported feeling more in control and empowered. The new systems delivered transparency, allowing gaps in provision to be quickly identified and addressed collaboratively.
Lindsey Scarisbrick, Clinical Lead for Endoscopy Services at UHMB, noted: ‘The outcome has meant faster access to diagnostic investigations, supporting cancer pathways and influencing a faster process from referral to treatment. This creates a positive patient experience and enhanced clinical outcomes.’
Sustaining the improvements
The beauty of focusing on systemic changes is their sustainability. The new relationships, transparency, skills, and improved systems foster an ongoing framework for maintaining and building upon the recovery. The project has since been expanded to other Trusts in the region, demonstrating its scalability and long-term value with significant results:
- 21% regional activity increase, translating to 8,709 additional patients treated annually;
- 27% reduction in waiting lists;
- £4.9mn in cost avoidance;
- 78% reduction in breaches at one Trust; and
- Improved appointment availability and planning visibility.
The way forward
As the NHS continues to contend with cancer backlogs, it’s crucial to resist the temptation of quick fixes. While additional funding is necessary, it must be coupled with fundamental operational improvements to yield lasting results.
The UHMB case study demonstrates that by focusing on the building blocks—the framework upon which a cancer service runs—we can establish systems that are robust in times of both calm and crisis. This approach not only addresses immediate backlogs but also builds resilience against future challenges.
As we move forward, let’s shift our focus from letting backlogs drive reactive behaviour to creating systems that inherently promote efficiency, quality care, and staff wellbeing. By doing so, we can build an NHS that is not just recovering from crisis but thriving in providing world-class care for all patients, regardless of external pressures.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.