NHS England has introduced a new therapy (Burosumab) that hopes to transform the lives of hundreds of adults living with X-linked Hypophosphatemia (XLH), a rare genetic disorder that causes severe bone, dental, and skeletal issues
The therapy, Burosumab, is now available to eligible adults across more than 20 specialist centres in England. It has already been available for children since 2018 and has proven to significantly improve bone health, reduce pain, and enhance mobility for those living with this debilitating condition.
Treating XLH in adults
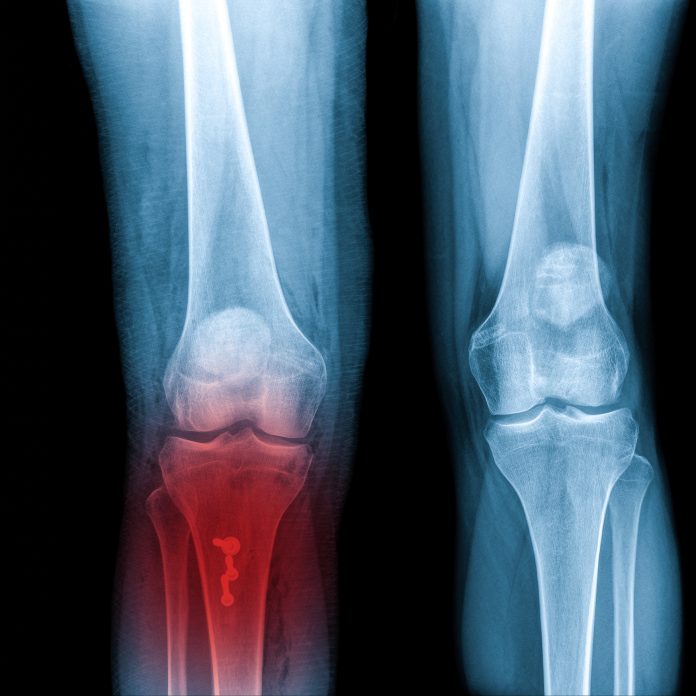
XLH is a genetic disorder that leads to low phosphate levels in the blood, a mineral essential for healthy bones and teeth. Phosphate deficiency disrupts bone formation and can result in rickets, an increased risk of fractures, muscle weakness, and dental problems like abscesses and tooth loss. Patients often experience chronic pain and, in severe cases, mobility issues, leading to disability that can affect their professional and personal lives.
Until the NHS released this new therapy, adults with XLH had limited treatment options. The main treatment included phosphate supplements and activated vitamin D, both of which offered only limited benefits and were associated with side effects such as stomach problems and kidney stones.
Burosumab, however, works differently by directly targeting the hormone responsible for phosphate loss, stabilising phosphate levels in the blood. This mechanism of action has shown to be far more effective than previous therapies.
The launch of burosumab for adults marks a significant step forward in the treatment of XLH, offering patients a much-needed alternative that addresses the root cause of the condition.
Reducing the need for NHS appointments
The drug helps stabilise phosphate levels but also accelerates bone healing, reduces pain, and decreases the need for invasive surgeries. This treatment is especially beneficial for adults who suffer from frequent bone fractures that might otherwise require surgical intervention. By improving bone strength and reducing fracture healing times, burosumab offers patients the possibility of avoiding long-term disability.
One of the main advantages of burosumab is its potential to reduce the need for hospital visits. Patients will be trained by NHS staff to administer the treatment at home, which will help reduce the number of trips to hospitals and allow individuals to continue with their daily lives with minimal disruption. This home-based approach not only improves the convenience of treatment but also ensures that patients have a more comfortable experience, giving them greater control over their health management.
The new treatment has been supported by the medical community as a game-changer for adults with XLH. The National Institute for Health and Care Excellence (NICE) has endorsed using burosumab as both a clinically effective and cost-effective therapy for XLH, making it available to a larger group of patients.
Improving the lives of people with XLH
With NHS funding now confirmed, the treatment is expected to significantly improve the quality of life for individuals suffering from this rare condition.
Patients who have struggled with chronic pain and limited mobility are already reporting marked improvements in their condition. Within just a few months of starting treatment, many have reported reductions in pain, enhanced energy levels, and improved physical function. For some, the changes have been so profound that they have regained the ability to engage in everyday activities, such as shopping, travelling, and even going on long trips, without the debilitating pain that previously held them back.
The roll-out of burosumab in England is a significant milestone for the XLH community and a testament to the NHS’s commitment to providing innovative, life-changing treatments for rare conditions. By offering a therapy that addresses the root cause of XLH, the NHS is improving bone health and also enhancing patients’ overall well-being and quality of life.
The availability of burosumab on the NHS is expected to bring long-term benefits, both for individual patients and the broader healthcare system.
The treatment offers an opportunity to reduce the burden on emergency services and long-term care by preventing complications such as fractures, surgical interventions, and chronic pain management.