The Council of European Dentists (CED) is a not-for-profit association representing over 340,000 dentists. Here, they address the relationship between oral health and overall health, as well as the necessary steps to improve access to dental care and reduce related inequalities
Dental healthcare remains at the forefront of advancing oral health in the European Union, with 4,7% of the EU population aged 16 years or over having an unmet need for dental treatment or examination (Eurostat, 2023).
Poor oral health is illustrated in all EU countries by remaining inequalities, both in terms of the prevalence of oral diseases and the level of accessibility of population groups to comprehensive oral and dental healthcare services, including prevention and treatment. Half the European adult population is currently affected by oral health diseases, according to the World Health Organization. This includes dental caries, periodontal diseases, particularly prevalent among lower socioeconomic classes, oral cancer, and tooth loss. The Council of European Dentists is the main body representing the dental profession at the European level, covering over 340,000 dentists from 31 countries. What role should dentistry and oral health, therefore, play in the overall improvement of general health?
Interlinkages between oral health and general health
Oral and dental health inequalities can be measured by various indicators, including socioeconomic, cultural, and commercial determinants of oral health, the level of availability, accessibility, acceptability, and high quality of care, and finally, the level of population coverage. Coverage can here be understood as the different strands of the population covered, specific services covered, and finally, economic costs covered.
As reasserted over the years, strong evidence-based research has shown the importance of considering poor oral health hand in hand with a broader angle of a patient’s health, and thus for several reasons:
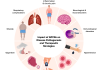
- Causal relationship between oral diseases and other diseases: Oral health and general body health are closely interlinked. Examples of diabetes, stroke, cardiovascular diseases (CVD), high blood pressure, adverse pregnancy outcomes, respiratory diseases, and dementia, as well as Human Papillomavirus infections (HPV) and other non-communicable diseases, may impact oral and dental health and be caused or further deteriorated by pre-existing oral health conditions such as periodontal disease and primary gum infections.
Furthermore, prescribed treatments for oral and general diseases may impact and affect each other. Some medications can, therefore, cause xerostomia, a reduced flow of saliva leading to a dry mouth, slow healing, and oral surgical complications, as well as increased risk of oral diseases such as periodontitis and tooth decay, more commonly detected in older patients.
- Common risk factors: Several risk factors of oral diseases, such as sugar, tobacco and alcohol, are common to major chronic non-communicable diseases. These disproportionately impact lower-income and disadvantaged European communities.
- Prevention and monitoring of diseases: Oral health monitoring of patients is also a strong and effective tool for the surveillance, prevention and detection of other health conditions. The early detection and diagnosis of signs of Human Papillomavirus (HPV) infection and related oropharyngeal cancers can and should systematically be carried out by dentists during routine or treatment dental visits. Early detection has indeed the potential to increase cancer survival rates by up to 30% compared to late detection.
Therefore, it is essential that the role of systematic dental check-ups is acknowledged and included in European health policies and programmes for disease surveillance and prevention.
Disparities in dental and oral care access
Most European states currently have public healthcare systems that deliver at least some level of oral healthcare coverage. However, statutory coverage for dental care, including more extensive dental treatments, diverges from country to country. Dental out-of-pocket payments, therefore, remain an important share of personal healthcare expenditures for individuals, impacting, more importantly, those with lower purchasing powers.
Although more extensive data is needed, the barriers to accessing high-quality dental and oral care are significantly more important for key disadvantaged and vulnerable groups.
The CED is renewing its call on EU policymakers to accelerate and prioritise prevention in relation to oral health. This includes the urgent need to pay specific attention to key social groups, including commonly excluded populations from existing national programs that aim to cover essential and preventative oral care services. The most common national programmes mainly target children and young adults in an effort to focus on preventative healthcare.
Successful outcomes of implemented programmes demonstrate the need to extend them to other social groups (including older adults, people with disabilities, migrant populations and asylum seekers, and socially disadvantaged and minority communities) and ensure an appropriate number and well-equipped workforce for the effective running of services.
National policies should, therefore, accelerate the implementation of Universal Health Coverage by including oral healthcare into existing benefit packages of national health systems. This would significantly help reduce the social, economic, and general health burden of mostly preventative oral diseases.
Dentistry and AMR reduction strategies
Socioeconomic inequalities in health and oral health are also recognised as significantly impacting the level of exposure to AMR and widening existing inequalities.
Dentistry remains responsible for 10% of prescribed antibiotics. Dental practitioners have a significant role in contributing to decelerating the spread of antimicrobial resistance (AMR) in Europe. This role is consistent with the link between oral and general health and preventing and slowing other health conditions through performed dental and oral treatments.
Therefore, the CED welcomes the launch of the second edition of the European Joint Action for AMR reduction, JAMRAI 2. The CED looks forward to renewed and strengthened collaboration between European dental professionals, other healthcare professionals, and the wider health sector.
The CED also calls on EU policymakers under the 2024 CED Manifesto to develop effective policy strategies for responsible antibiotic use to combat AMR through close collaboration with the dental profession. This comprises accelerating antimicrobial stewardship, continued education and awareness, effective infection control and prevention (ICP) measures, inter-professional cooperation and integrated care.
At the start of the new EU mandate, renewed attention needs to be paid to tackle and reduce oral health inequalities, which is essential to improve European general health. Improved communication and collaboration across healthcare sectors, including among dentists, doctors, nurses, and other healthcare professionals, ensures the delivery of integrated and holistic care. Let’s help improve oral health and reduce the burden of chronic and non-communicable diseases in Europe.