A recent report by The Lancet Diabetes & Endocrinology Commission calls for a shift in obesity diagnosis, proposing a more comprehensive and clinically relevant approach
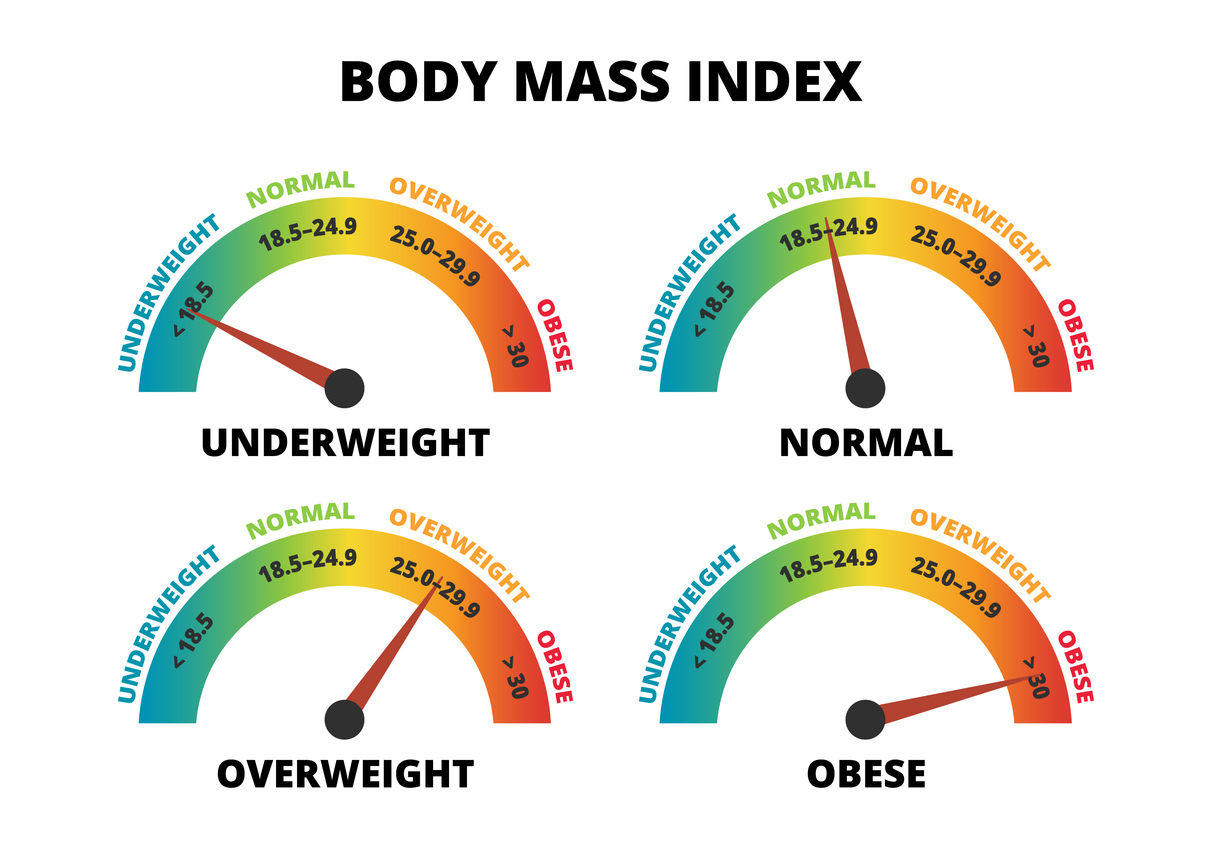
For decades, Body Mass Index (BMI) has been the go-to metric for diagnosing obesity. However, BMI is a blunt tool that doesn’t distinguish between fat and muscle, fails to consider fat distribution, and overlooks critical signs of health or illness. This has led to widespread under- and over-diagnosis of obesity, misinforming patients and leaving many at risk.
Why current BMI-based obesity diagnosis falls short
- Lack of precision: BMI measures body weight relative to height but does not differentiate fat from muscle.
- Example: Athletes with high muscle mass often receive false-positive obesity diagnoses.
- Inadequate Risk Assessment: Obesity’s health risks stem from fat’s effects on organs, which BMI cannot assess.
- Ethnic discrepancies: BMI thresholds vary across ethnicities, rendering “one-size-fits-all” metrics inadequate.
A new framework: preclinical vs. clinical obesity
To address these limitations, the Commission introduces two new categories:
Preclinical obesity:
- Defined as excess body fat without ongoing illness.
- Individuals remain functional but face elevated risks of future diseases such as Type 2 diabetes, cardiovascular issues, and clinical obesity.
Clinical obesity:
- A chronic condition where excess fat impairs organ function or daily activities.
- Associated with symptoms like breathlessness, joint pain, or metabolic abnormalities.
A more comprehensive diagnosis process
Health professionals are encouraged to shift focus from BMI to a three-step diagnostic approach:
- Confirm excess fat: Use waist circumference, waist-to-hip ratio, or advanced scans (e.g., DEXA) to assess fat levels.
- Assess health impact: Evaluate symptoms of organ dysfunction (e.g., kidney issues, mobility limitations).
- Establish the root cause: Determine whether observed dysfunctions are obesity-related.
- Personalised management strategies.
Preclinical obesity:
- Focus on prevention through health counseling and weight stabilisation.
- Active weight-loss interventions for high-risk patients.
Clinical obesity:
- Treat organ dysfunction through targeted interventions.
- Success should be measured by functional improvement, not weight loss alone.
Implications for stakeholders
For healthcare providers:
Transitioning to the proposed model will require additional training in advanced diagnostic techniques and patient-centered care.
For payers and policymakers:
Adopting evidence-based frameworks can optimise healthcare costs by focusing on prevention and tailored interventions.
For businesses (e.g., pharmaceutical, wellness companies):
The demand for tools like DEXA scanners, wearable health monitors, and personalised treatments is likely to grow.
A step forward in combating obesity
This new approach marks a shift from treating obesity as a one-dimensional condition to addressing it as a spectrum of health risks and illnesses. By embracing this model, healthcare professionals can provide more precise, effective, and compassionate care, ensuring better outcomes for patients.