Cancer cells are masters of disguise, evading immune destruction through cunning mechanisms. Groundbreaking research reveals a novel tactic: mitochondrial transfer.
Cancer cells cripple immune cells by donating their damaged mitochondria, hindering the immune response and fostering tumour growth
The immune system is a powerful defence against cancer, programmed to recognize and destroy malignant cells. However, cancer cells are adept at evading this surveillance, developing sophisticated mechanisms to escape immune attack.
Understanding these evasion tactics is crucial for developing more effective cancer immunotherapies. Recent research from Okayama University, Japan, has uncovered a novel mechanism by which cancer cells manipulate the immune system: by transferring their mitochondria to immune cells, effectively crippling their ability to fight the tumour.
This groundbreaking discovery sheds light on the complex interplay between cancer and the immune system and offers potential new avenues for therapeutic intervention.
Mitochondrial transfer: A key immune evasion strategy
The tumour microenvironment (TME), the area surrounding a tumour, is a complex ecosystem where cancer cells interact with immune cells. Cancer cells can manipulate the TME to their advantage, weakening tumour-infiltrating lymphocytes (TILs), the immune cells designed to target and destroy the tumour. Mitochondria, the cellular powerhouses responsible for energy production, play a critical role in the metabolic reprogramming of both cancer cells and TILs. However, the precise mechanisms by which mitochondrial dysfunction contributes to immune evasion have remained poorly understood.
In collaboration with researchers from the Chiba Cancer Center Research Institute, Professor Yosuke Togashi and his team at Okayama University have made a significant breakthrough in this area. Their research, published in Nature, reveals that cancer cells can transfer their mitochondria to immune cells, which significantly impairs the immune response. “We have discovered mitochondrial transfer as one of the key mechanisms of immune evasion,” explains Professor Togashi.
“Our research adds a new dimension to the understanding of how tumors resist immune responses, potentially leading to the development of more comprehensive and tailored approaches in treating different cancers.”
The Mechanics of Mitochondrial Manipulation
Mitochondria possess their own DNA (mtDNA), which encodes proteins essential for energy production. However, mtDNA is susceptible to damage, and mutations in mtDNA can actually promote tumour growth and metastasis. The researchers discovered that TILs within the TME often harbour the same mtDNA mutations as the cancer cells themselves. Further investigation revealed that these mutations were linked to abnormal mitochondrial structures and dysfunction within the TILs.
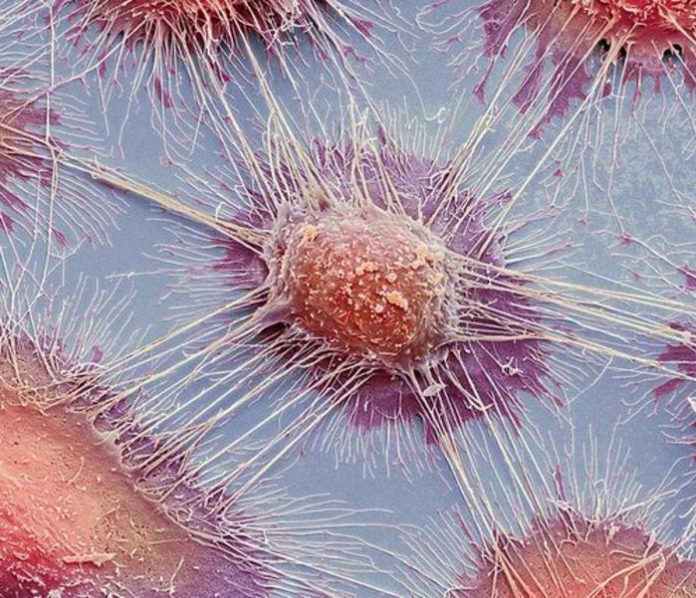
Using fluorescent markers, the team tracked the movement of mitochondria between cancer cells and T cells. They observed that mitochondria were transferred through direct cell-to-cell connections called tunnelling nanotubes, as well as via extracellular vesicles. Once inside the T cells, the cancer-derived mitochondria gradually replaced the T cells’ original mitochondria, a process known as ‘homoplasmy.’
Disrupting Mitophagy and Impairing Immune Response
Often, damaged mitochondria in TILs are removed through a process known as mitophagy. However, the mitochondria transferred from cancer cells appeared to resist this degradation. The researchers discovered that factors inhibiting mitophagy were co-transferred along with the mitochondria, preventing their breakdown.
This led to mitochondrial dysfunction in the TILs, resulting in decreased cell division, metabolic alterations, heightened oxidative stress, and an impaired immune response. In mouse models, these dysfunctional TILs also showed resistance to immune checkpoint inhibitors, a common type of immunotherapy.
Therapeutic implications
The discovery of mitochondrial transfer as a novel immune evasion mechanism opens up exciting new possibilities for cancer treatment. Blocking this transfer could potentially enhance the effectiveness of immunotherapy, especially in patients with cancers resistant to current treatments. “Existing cancer treatments are not universally effective, and there is a pressing need for new therapies that can overcome resistance mechanisms,” says Professor Togashi. “Developing drugs that inhibit mitochondrial transfer between cancer cells and immune cells may enhance the efficacy of immunotherapies, thereby providing personalized treatment options for patients with cancers resistant to current therapies.”
Cancer therapies often come with high costs and significant side effects, especially when they prove ineffective. By inhibiting mitochondrial transfer, the success rate of immunotherapy could be improved, reducing the burden of cancer and improving patient outcomes. This discovery not only provides crucial insights into cancer biology but also paves the way for the development of more targeted and effective cancer therapies in the future. Further research will be essential to translate these findings into clinical applications and bring new hope to cancer patients.










