Interoperability in healthcare is the ability to share and use patient information across different healthcare systems. In the NHS, this is vital for improving patient experience and comprehension
When systems work together smoothly, patients receive consistent and personalised information, which helps them better understand their care and feel more satisfied. Interoperability’s importance extends beyond administrative efficiency. It plays a critical role in clinical decision-making, enabling healthcare providers to access up-to-date patient records, previous medical history, and real-time health data. This comprehensive view helps doctors make informed decisions quickly, reducing the chances of errors and improving patient safety. As the NHS continues to embrace digital transformation, the need for seamless data integration becomes even more crucial to meet the growing demands of patient care.
A patient’s journey: The impact of inconsistent communication 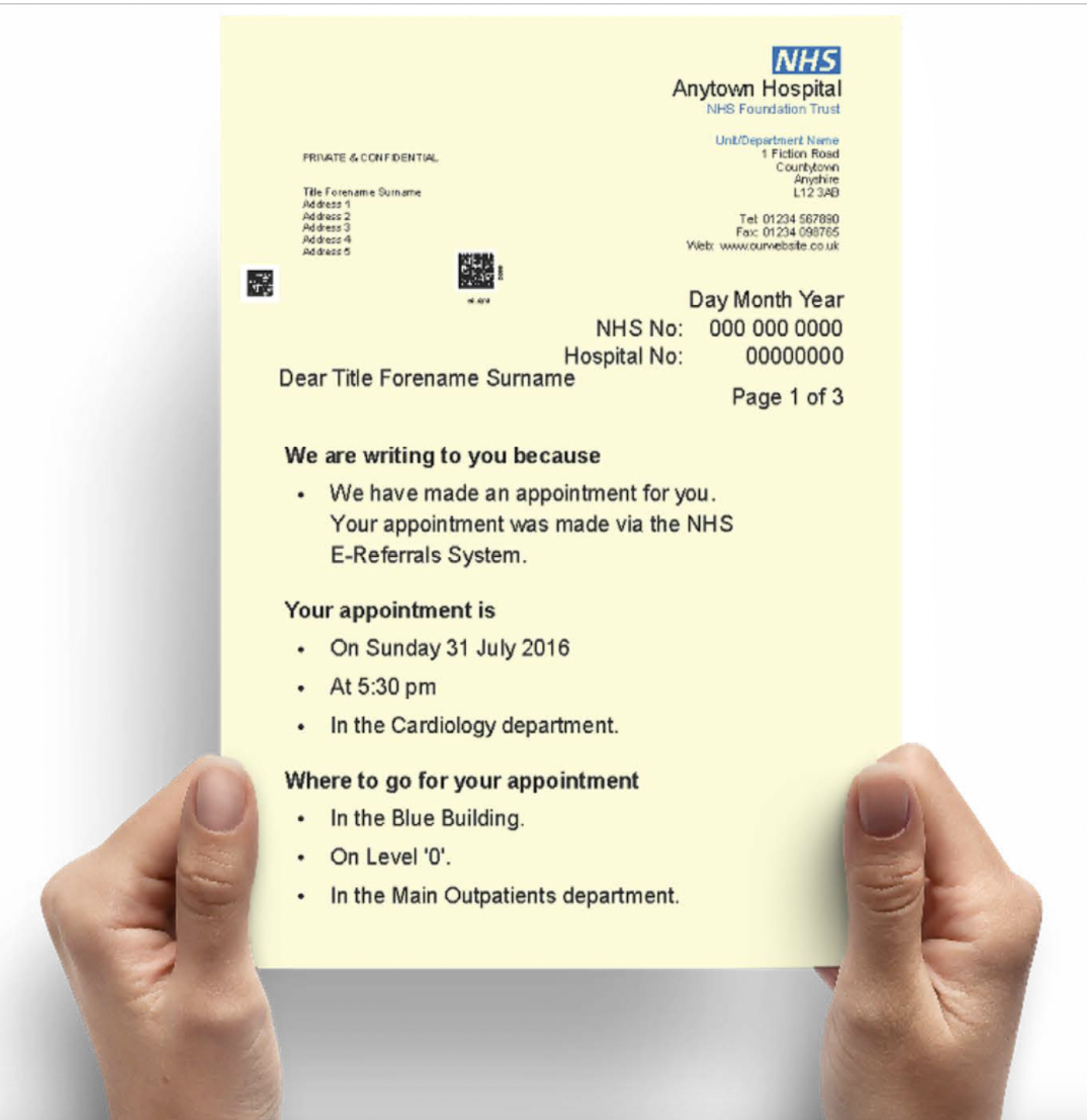
If we are to put ourselves in the perspective of a patient with dyslexia, they may need written communications printed on yellow paper to read easily. They may inform the hospital staff, and their next outpatient letter will arrive printed on the requested yellow paper. However, when referred to another department, the next letter comes on standard white paper. The patient struggles to read it and understand the details, and then doesn’t know what is being asked of them, so they either discard the letter or call the hospital to ask what they are meant to do.
This inconsistency can cause frustration. Patients who can’t understand appointment details may feel overlooked and not prioritised, leading to a low satisfaction in their patient experience. It can also lead to missed appointments because of confusion. Missed appointments affect patient health and put extra strain on NHS resources. These situations can create a cycle of disengagement, where patients feel less inclined to attend appointments due to recurring communication barriers. This, in turn, affects their health outcomes and can lead to the worsening of conditions that might have been managed more effectively with timely care, and may also lead to further missed appointments due to patients not having trust in their healthcare.
The financial implications of missed appointments are substantial. Each missed GP appointment costs the NHS an average of £30, amounting to approximately £216 million annually across England. In secondary care, the costs are even higher; for instance, each missed hospital outpatient appointment is estimated to cost around £120. Collectively, missed hospital appointments cost the NHS nearly £1 billion over a four-year period. These figures underscore the critical need for consistent and accessible patient communication to mitigate missed appointments and their associated costs. These costs could be reduced through the improved interactions between systems and data sharing, which would mean that gaps in patient pathways are not missed, and NHS staff are provided with a more well-rounded view of the patient.
The emotional toll on patients should not be underestimated. Feeling ignored or marginalised because of unaddressed accessibility needs can break their trust in the healthcare system. For patients with chronic conditions or disabilities, consistent communication tailored to their needs is essential for maintaining continuity of care. A 2022 survey found that overall satisfaction with the NHS fell to 29%, the lowest level since the survey began in 1983. The main reasons for dissatisfaction included long waiting times and staff shortages. However, accessibility and the ease of understanding health communications also significantly shape patient perceptions.
The challenges of achieving interoperability in the NHS
Interoperability isn’t just a tech issue. It involves organisational structures, old systems, and differing priorities across NHS trusts. Many NHS systems work in isolation. This leads to repeated efforts, inconsistent records, and patients having to fill the gaps themselves. The lack of a unified approach often results in fragmented care, where critical patient information is lost between departments, affecting the quality of treatment. Different IT systems are a big challenge. NHS trusts use various software that doesn’t always connect well. Data standardisation is another issue that pairs with this and causes issues. Departments may use different coding systems, making it hard to merge patient information. This can cause vital data to be lost or miscommunicated. Without standardised data formats, interoperability becomes a patchwork solution, where some systems communicate effectively while others remain isolated. This means that it’s important to work on ensuring that all departments are using the same coding systems, which will, in turn, make comprehension easier for NHS staff and improve the patient experience.
Budget constraints make things harder, as updating systems costs money. Training staff also requires time and resources. Limited budgets often delay upgrades, leaving outdated systems in place. This situation is compounded by competing priorities within NHS trusts, where immediate clinical needs may take precedence over long-term IT investments. Concerns about data privacy and security can slow things down, too. NHS trusts must follow strict rules to protect patient data, which can create additional layers of complexity when implementing new interoperable systems. The greatest way of addressing this is to attempt to manipulate and transform the data so that differing systems can work alongside one another but be connected via data streams that can automatically do this work for them.
Additionally, the human factor cannot be ignored. Resistance to change is common in large organisations, and the NHS is no exception. Healthcare professionals may be hesitant to adopt new technologies, especially if they perceive them as disruptive to established workflows. Effective change management strategies are essential to ensure that staff are engaged, trained, and supported throughout the transition to interoperable systems. The commitment to interoperability is one that needs buy-in from many areas but also requires consistency and support throughout to achieve the desired success of implementing this change.
Addressing the interoperability challenge
Despite these hurdles, the NHS can greatly improve interoperability to greatly enhance patient experience. Moving towards open standards is key. When systems use the same data protocols, sharing information becomes far easier and enables more connect between departments. Open standards ensure that data can flow seamlessly between different systems, regardless of the software vendor or platform.
Investing in digital platforms can help. These platforms allow real-time data sharing. They reduce errors and ensure patient preferences—like using yellow paper—are respected across departments. Integrated digital platforms can consolidate patient information from multiple sources, providing healthcare professionals with a comprehensive view of a patient’s medical history, treatment plans, and ongoing care needs.
Collaboration is also important. IT vendors, healthcare providers, and policymakers must collaborate to find the best solutions. Public-private partnerships can drive innovation and help the NHS leverage cutting-edge technologies without bearing the full financial burden. Engaging with patients and advocacy groups can also provide valuable insights into the specific needs and expectations of different patient populations.
Strong data governance builds trust. It ensures data is secure while allowing information to flow where it’s needed. Clear policies and robust security measures can mitigate risks associated with data breaches and unauthorised access. Training NHS staff to use new systems effectively is just as important, as these people are at the heart of making these changes work. Continuous professional development programs can equip healthcare professionals with the skills to navigate new technologies confidently and prepare for future technological developments that could further improve processes, such as Artificial Intelligence (AI). When new technologies do appear, there are undoubtedly risks, so development training and awareness are incredibly important for all staff.
Technologies offer more opportunities. Software can be used to help connect these data streams, taking the burden of data transformation away from the NHS itself. This is especially important as it would mean that, rather than all moving to specific systems, the systems will be able to interact with one another and provide a seamless approach with minimal changes to the staff. Cloud-based solutions, for example, can facilitate data sharing across geographic and organisational boundaries, supporting integrated care models and improving patient outcomes.
As mentioned, emerging technologies such as artificial intelligence and machine learning can enhance interoperability further. AI can analyse vast amounts of health data to identify patterns, predict patient risks, and support clinical decision-making. Predictive analytics can help healthcare providers anticipate patient needs, reduce hospital readmissions, and optimise resource allocation.
Interoperability in the NHS is more than a tech upgrade. It’s about transforming healthcare to meet patient needs better. Consistent, accessible communication can greatly improve patient satisfaction and health outcomes. By tackling interoperability challenges, the NHS can build a more integrated, efficient, and patient-focused system. This will reduce missed appointments and raise the quality of care. The journey is complex, but with the right investment and collaboration, the NHS can achieve healthcare excellence.
Ultimately, achieving interoperability is not just a technical goal but a strategic imperative for the NHS. It requires a cultural shift towards embracing digital health innovations and prioritising patient-centred care. By fostering an environment of continuous learning, collaboration, and innovation, the NHS can create a future where every patient receives the right care at the right time, supported by seamless, secure, and efficient information exchange. This vision of interconnected healthcare systems holds the promise of improved health outcomes, greater patient empowerment, and a more resilient NHS for generations to come.
How Synertec ’s Prism Software enables interoperability
Synertec’s expertise in document control and communication solutions uniquely addresses the interoperability challenges faced by the NHS. Their software, Prism, unifies disparate systems and streamlines communication processes, creating a cohesive system where information flows seamlessly across platforms and care settings.
Prism supports interoperability by interacting with existing systems, it can accept work from any host system and information format, ensuring that critical patient information is accurately captured, transformed, and delivered to the recipients at the right time. In turn, this reduces errors and improves efficiency. Prism can be tailored to meet the specific needs of NHS Trusts and other healthcare organisations, aligning with key priorities such as meeting the Accessible Information Standard, digitalisation of processes, and compliance with data protection regulations.
By leveraging Prism, the NHS can enhance patient engagement and experience through more effective sharing of information across departments and to its patients.