L. Maximilian Buja, MD, Professor of Pathology and Laboratory Medicine at McGovern Medical School, The University of Texas Health Science Center at Houston, turns the spotlight onto medical education both past and present
The traditional medical education system, widely adopted throughout the twentieth century after the 1910 Flexner report, has produced generations of scientifically grounded and clinically skilled physicians, as well as subsets of academic physicians and physician-scientists who collectively have served medicine and society well. The Flexnerian undergraduate medical education (UME) curriculum is comprised of a distinct pre-clinical component with subject-based courses in the foundational sciences and a subsequent clinical clerkship component in the major medical specialities.
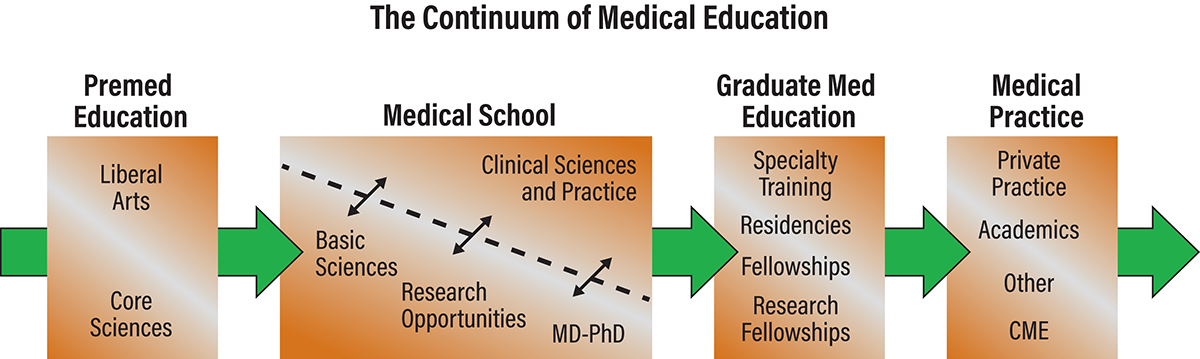
Over the years, modifications have been made to promote integration of the two components (Figure 1). This UME education provides the basis for subsequent graduate medical education (GME) training and a professional career enhanced by continuing medical education and lifelong learning (Buja 2019).
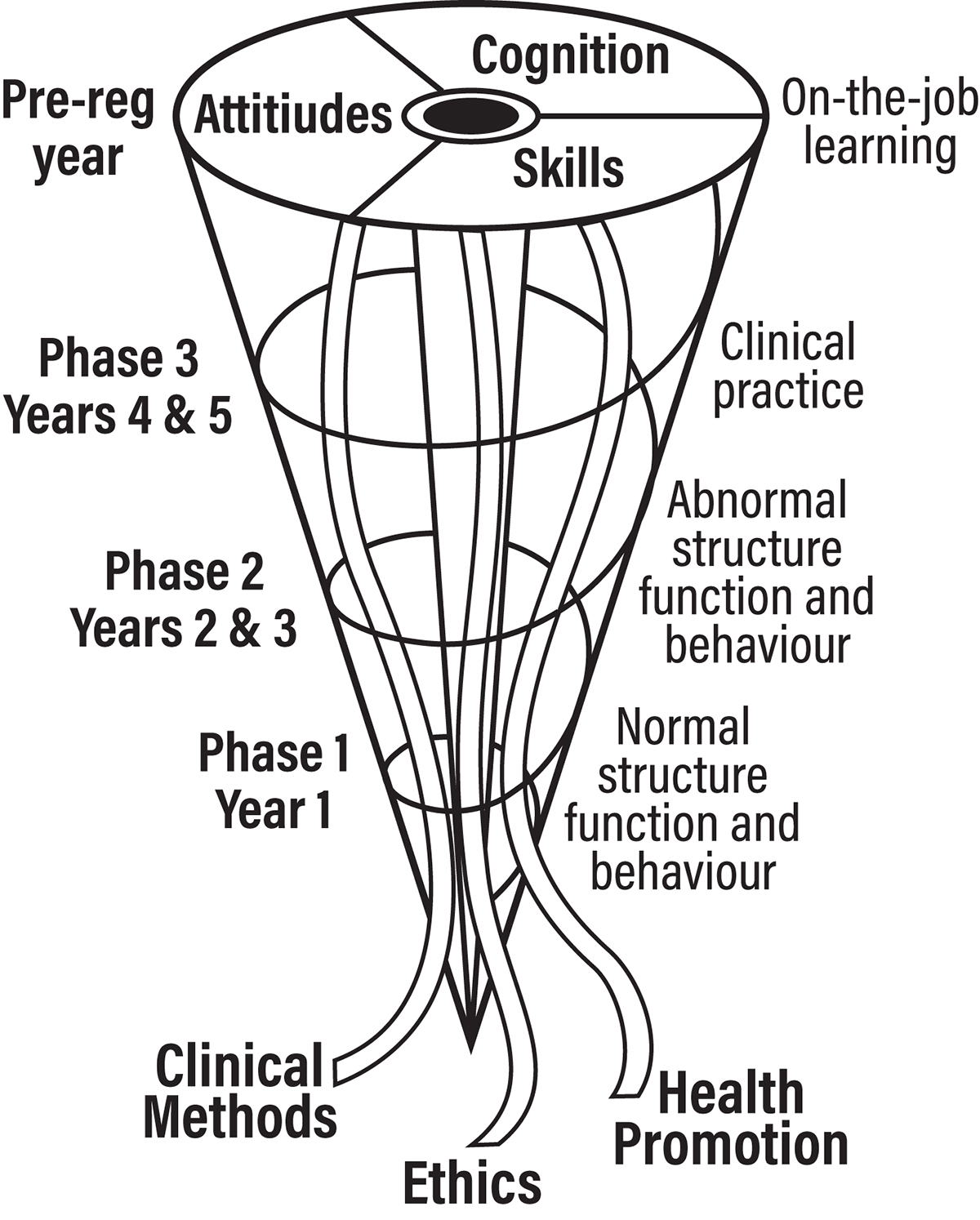
Yet, in response to criticisms of the traditional system and changes in the healthcare landscape, sweeping changes were launched constituting a revolution in UME and GME (Irby and O’Brien 2010). The core goal of the post-Flexnerian construct is the production of physicians “fit for the twenty-first century.” The emphasis is on developing skills in modern clinical reasoning and decision-making. The construct to achieve this overarching goal is the so-called fully integrated spiral curriculum encompassing both horizontal and vertical integration across time and across disciplines (Figure 2). The new curricula fit the definition of “disruptive innovation.” Whereas innovation is generally perceived as being good or making improvements, disruptive innovation is prone to risks and unintended consequences (Neem 2017).
Re-engineering the curriculum
Curriculum designers have reconstructed the content of the curriculum as well as pedagogical methods geared to the learning styles of contemporary students, with a major increase in faculty and staff in order to deliver content in smaller groups than in a lecture format. (Twenge 2009). The lecturer now is being reprogrammed as a learning facilitator, creating stress for many faculties.
The fully integrated curriculum resulting from the redesign does away with the distinction between the critically important pre-clinical (basic medical sciences) two-year period and the apprenticeship-like clinical two-year period. It brings in additional content called Health Systems Science, as a co-equal to basic and clinical sciences, to cover topics from population health to interdisciplinary care. There has also been a push in recent years for undergraduates to demonstrate “competencies” rather than cognitive knowledge. The result of these initiatives has been a repeal of a significant amount of time for the basic sciences curriculum.
Perspectives
Integration within the curriculum certainly has merit, but there are more effective ways to achieve that objective without sacrificing the foundations of a good medical education. The way forward is the repositioning of medical science in the medical education curriculum to reflect its unchanging and continued importance. While the restoration of subject-based foundational courses is unlikely to happen, there is an imperative to maintaining the integrity and cohesion of the foundational disciplines. This is especially true for pathology which fulfils the time-honoured roles of linking basic biomedical science to clinical medicine and providing an understanding of the pathological basis of disease. It is inevitable that the reduction of teaching in pathology absent from a coherent pathology course will have a significant untoward effect on a physician’s clinical acumen and expertise. Studies have repeatedly shown that factual knowledge of medical science is essential for the development of clinical skills.
It is also important to counter the undue influence United States Medical Licensing Exam (USMLE) Step 1, as the sole objective evaluator of medical students’ cognitive achievement creating an adverse “Step 1 climate” in the preclinical years (Chen et al 2019). The recent decision of the National Board of Medical Examiners to make the USMLE a pass/fail exam without reported numerical score is well-intended. However, a definitive solution requires a return to providing meaningful grades for courses and an overall rigorous summative evaluation for the four years of medical school.
Whereas there is merit in the goal of the new curricula to produce holistic physicians, a legitimate concern is that the new approach will produce graduates who do not have the level of expected clinical expertise because they do not have a grounding in biomedical science or a deep understanding of the pathological basis of disease. Enthusiasm for reform needs to be tempered by a more cautious and realistic approach to avoiding unintended consequences.
Please note: This is a commercial profile
References
Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach. 2015;37(4):312–322. doi:10.3109/0142159X.2014.970998
Buja LM (2019). Medical education today: all that glitters is not gold. BMC Medical Education 19:110-121. https://doi. org/10.1186/s12909-019-1535-9.
Chen DR, Priest KC, Batten JN, Fragoso LE, Reinfield BI, Laitman BM (2019). Student Perspectives on the “Step 1 Climate” in Preclinical Medical Education. Acad Med.94:302–4.
Irby CM, O’Brien BC (2010). Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Acad Med. 85:220–7.
Neem J (2017) The downside of innovation and disruption. Inside Higher Ed. https://www.insidehighered.com
Twenge J. (2009) Generational changes and their impact in the classroom: teaching generation me. Med Educ. 43:398-405. doi: 10.1111/j.1365-2923.2009.03310.x.