Here, Business Development Director at Aire Logic, Rob Hurrell, explains how COVID-19 has helped us all to become agile and deliver better digital health solutions, faster
It is fair to say that the world has changed dramatically over the past few months. Unless you can remember the last World War, nobody will have experienced such far-reaching changes to everyday life in such a short space of time.
COVID-19
A global pandemic has touched every aspect of how we live, work and communicate, giving new insight into each other’s lives as our personal and professional lives have merged. Many of us are now meeting and collaborating remotely in ways we could not have imagined (and, indeed, some argued were impossible) before a global pandemic made adoption of digital solutions essential, rather than a nice-to-have.
The NHS, of course, has pursued digital strategies for years as a route to reduce cost and improve patient care, but initiatives have often moved slowly with mixed results. One of the potential benefits of the COVID-19 response is that it has taught us a lot about what we can actually achieve when pressed. Not only is the NHS implementing technology solutions successfully, at speed, but we are finding in many cases that they offer the kinds of benefits sought for many years.
What’s changed isn’t necessarily the technology available, but the approach to developing and deploying solutions. As a health technology company, we have long-advocated the benefit of an agile methodology, working collaboratively with Trusts to establish requirements, deploy a Minimum Viable Product to provide immediate benefit, and layer additional functionality over time as requirements change. Strategic decisions by committee can be cumbersome and, with a situation such as COVID-19, the picture may change many times before there is agreement. It is far more important, therefore, to engage in an ongoing conversation with NHS Providers as the product is developed: ‘Here is the minimum viable product, how does this look? What else would you like to see included? Who should we make this available to?’ and so forth.
Situational Reporting
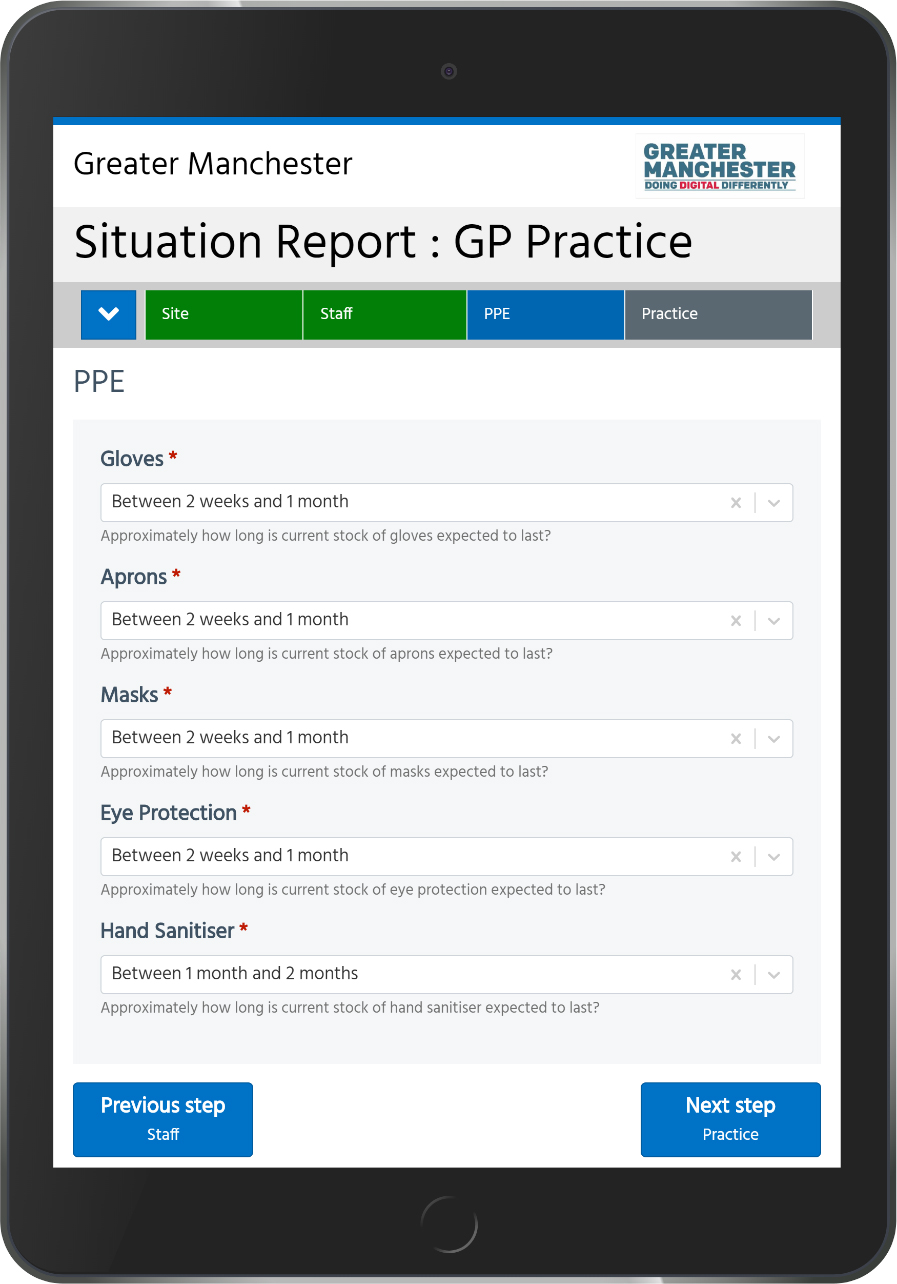
This is exactly the approach we took when we began working with Greater Manchester LHCRE to develop a Situational Reporting Tool to provide information on the status of NHS organisations in the region. They, in common with all providers, couldn’t easily say in advance what they needed; there was an awareness that Situational Reporting would be important, but no real template for what that might look like.
Combining advice from government bodies, NHS England and Healthcare providers in Greater Manchester, we were able to develop a Situational Reporting tool using a forms-based solution with some additional integrations to GM systems, in order to capture information on three key areas:
- Staff (total numbers, how many well, how many sick, clinical/non-clinical, etc.)
- PPE (Available gloves, aprons, masks, etc. with supply measured in days and weeks.)
- Status of service (OPEL Scoring from Green, or Capacity Available, through to White, or Service Suspended.)
This was initially deployed in a hospital context, but it soon became clear that the potential application was much wider, incorporating hospital care, community care, mental health Trusts, GP Practices, Dental Practices, and Pharmacies. For the solution to be able to offer any meaningful insight into the current situation and preparedness of these organisations, it was critical that we had good staff engagement in order to gather a large data set and that the questions asked (and responses collected) were relevant.
One of the early lessons we learned during this time was that, no matter how short we made the forms, understandably, staff who were already working at capacity became fatigued with filling them out over time and response rates dropped. We made a change to allow the solution to remember previous field entries so that respondents could make changes only where needed, and submission rates improved dramatically. Likewise, when ‘loss of sense of taste and smell’ was added to the list of COVID-19 symptoms on 18th May, we were able to incorporate this into the Greater Manchester solution almost immediately. The flexibility of the tool and our approach meant such changes could be implemented in hours, rather than days and weeks. With a situation which looked radically different from one day to the next, this responsiveness was key for any solution to remain viable and useful over time.
Of course, the real measure of success in any of this is the impact on health outcomes. Working with GM LHCRE stakeholders, we were able to collate SitRep data into a dashboard giving real insight into staff shortages and availability of PPE, and allowing for a significant redistribution of protective equipment and resources in the region to where they were most needed. This helped maintain service and reduce infection rates in clinical settings, potentially saving the lives of both staff and patients.
What are the lessons from all of this?
That, despite inevitable challenges which come from digitising workflows, rapid, agile solution development is possible in all settings, from GPs, to Hospitals, to Care Homes, and that the requirements of a technology solution can be driven as much by user feedback and engagement as they are by strategy and initial intentions.
COVID-19 has taught us how quickly we can innovate when we need to, and how instrumental technology can be in supporting healthcare functions. If this has been demonstrated in the space of two or three months in the midst of a global pandemic with the inevitable constraints that brings, it is encouraging to consider how we could progress digital health solutions in Healthcare in the months and years to come.
Please note: This is a commercial profile