Prof Dr Joost Sluijter, Professor, Cellular and Translational Cardiology at University Medical Center Utrecht shares an in-depth perspective on the needs for innovative treatments for heart failure
Concerning heart failure (HF), the current COVID-19 pandemic is having a dramatic effect on the daily life of each individual, ranging from social distancing measures applied in most countries to getting severely diseased due to the virus. Cardiovascular Disease (CVD) is among the most common conditions in people that die of the infection. The burden of CVD accounts for over 60 million people in the EU alone, therefore, it is the leading cause of death in the world.
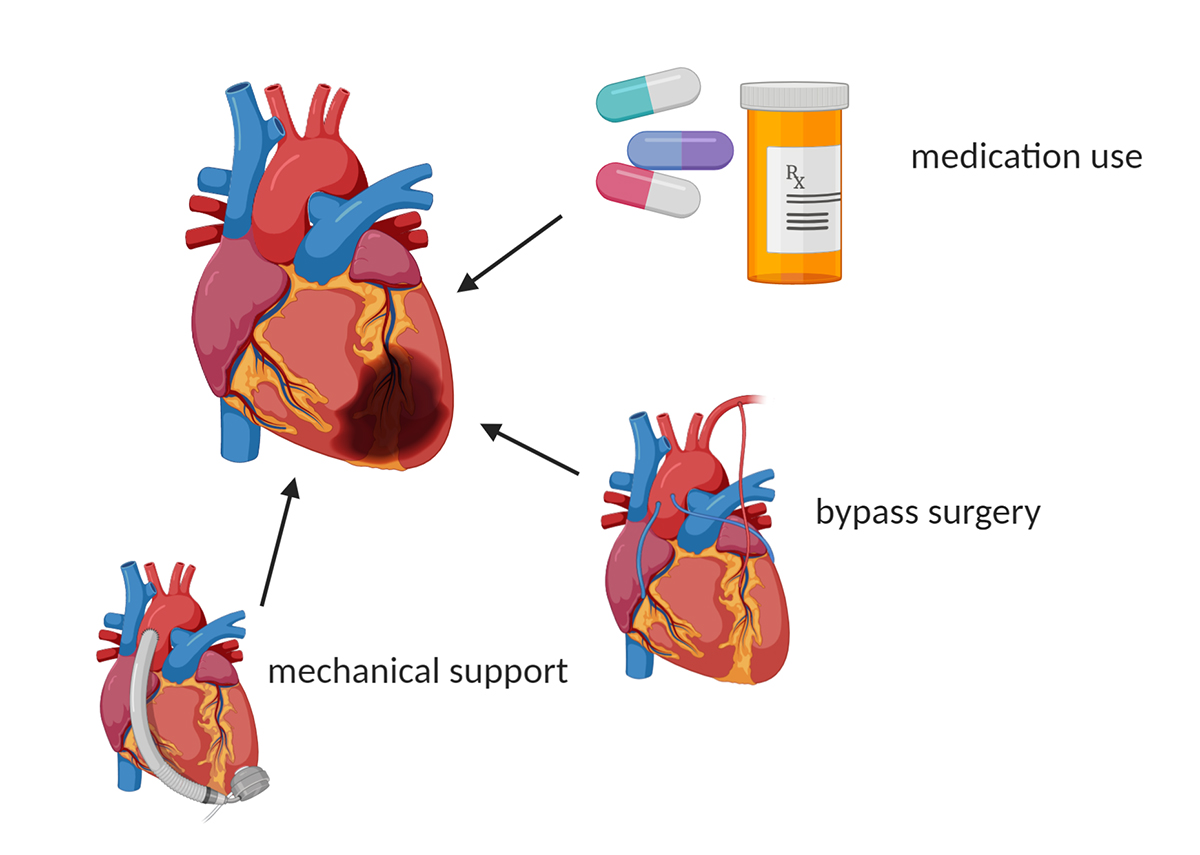
Although COVID-19 shows us the direct impact of a potential treatment for people’s health, CVD is a stealthy pandemic killer. HF is a chronic disease condition in which the heart is not able to fill properly or efficiently pump blood throughout your body, caused by different stress conditions including myocardial infarction, atherosclerosis, diabetes and high blood pressure. Several measures are commonly used to treat heart disease, such as lifestyle changes and medications like beta-blockers and ACE inhibitors, yet these typically only slow down the progression of the disease.
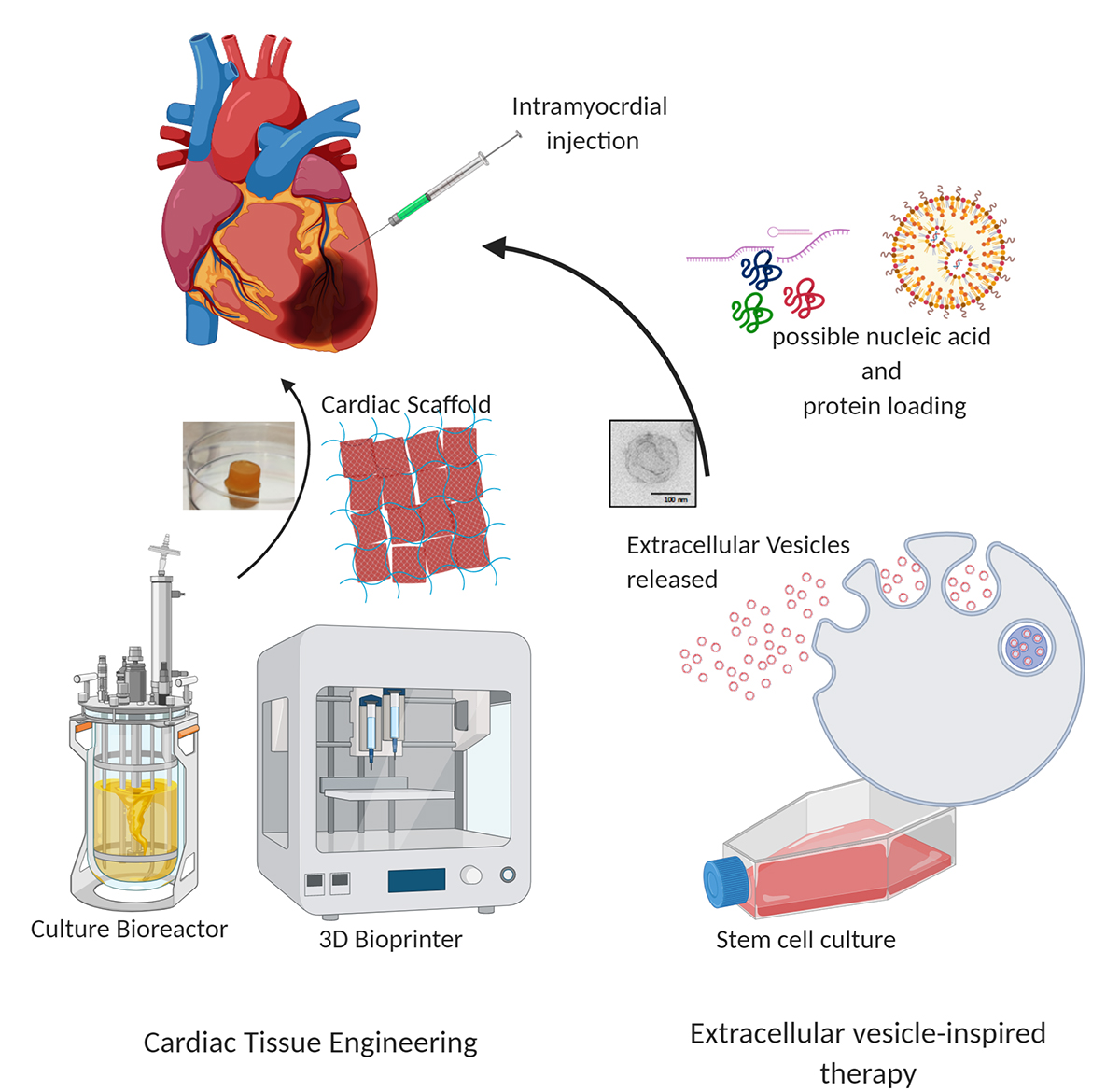
Biomedical research is exploring new avenues by combining scientific insights with new technologies to overcome chronic diseases like HF. Among the most appealing and promising technologies are the use of cardiac tissue engineering and extracellular vesicles-mediated repair strategies.
Cardiac tissue engineering
Upon an initial cell loss post-infarction, it is appealing to replace this massive loss in contractile cells for new cells and thereby not treating patients’ symptoms, but repairing the cause of the disease. Cardiac cell therapy has been pursued for many years with variable results in small initial trials upon injection into patients. Different cell types have been used to help the myocardium in need, but the most promising approaches aim to use induced pluripotent cells (iPS) from reprogrammed cells from the patient themselves that can be directed towards contractile myocardial cells. These cells in combination with natural materials, in which the cells are embedded in the heart, can be used for tissue engineering strategies (1). Together with different international partners, Sluijter’s team are trying to develop strategies to use these iPS-derived contractile cells for myocardial repair via direct myocardial injection (H2020-Technobeat-66724) or to make a scaffold that can be used as a personalised biological ventricular assist device (H2020-BRAVꓱ-874827). A combination of engineering and biology to mimic the native myocardium aims to replace the chronically ill tissue for healthy and well-coupled heart tissue that can enhance the contractile performance of the heart.
Recently, a Dutch national programme started, called RegMedXB, in which the reparative treatment of the heart is aimed to be performed outside the patient’s body. During the time the heart is outside the body; the patient is connected to the heart-lung machine, and after restoring function, it will be re-implanted. The so-called Cardiovascular Moonshot aims to create a therapy that best suits the individual patient, by having their heart beating in a bioreactor, outside the body. Although it sounds very futuristic, many small lessons will be learned to feet novel therapeutic insights.
Extracellular vesicle-inspired myocardial repair
The initial injection of stem cells did result in a nice improvement of myocardial performance. We have now learned that rather than these delivered cells helping the heart themselves, the release of small lipid carriers called extracellular vesicles (EVs) (2) from these cells occur. These EVs carry different biological molecules, including nucleotides, proteins and lipids, and are considered to be the bodies’ nanosized messengers for communication. The use of stem cell-derived EVs are now being explored as a powerful means to change the course of the disease. Via these small messengers, natural biologics are delivered to diseased cells and thereby help them to overcome the stressful circumstances. EVs carry reparative signals that can be transferred to the diseased heart and thereby change the course of heart disease in some patients.
Within the EVICARE program (3) (H2020-ERC-725229), Sluijter’s team are using stem cell-derived EVs to change the response of the heart to injury. Also, to understand which heart cells and processes are being affected, they use materials to facilitate a slow release of biomaterials over an extended period rather than a single dose, which is probably essential for a chronic disease like HF. For now, improved blood flow is the main aim but the team have seen other effects as well, such as cardiovascular cell proliferation (4) by which the heart cells themselves start to repair the organ.
Stimulating endogenous repair mechanisms
The use of EVs basically aims to enhance the endogenous repair mechanisms of the heart. These natural carriers can be mimicked with synthetic materials, or used as a hybrid of the two, thereby creating an engineered nanoparticle, that is superior in the intracellular delivery of genetic materials. The possibility of loading different biological materials allows a further tuning of its effectiveness and use in different disease conditions, creating a new off-the-shelf delivery system for nanomedicine to treat cancer and CVD (H2020-Expert-825828).
Conclusion
As is true of the current COVID-19 pandemic, HF is also a growing chronic disease that affects millions of people worldwide. The chronic damaged myocardium needs reparative strategies in the future to lower the social burden for patients, but also to keep the economic consequences affordable. New scientific insights with cutting edge technological developments will help to address these needs of CVD patients and their families.
References
(1) Madonna R, Van Laake LW, Botker HE, Davidson SM, De Caterina R, Engel FB, Eschenhagen T, Fernandez-Aviles F, Hausenloy DJ, Hulot JS, Lecour S, Leor J, Menasché P, Pesce M, Perrino C, Prunier F, Van Linthout S, Ytrehus K, Zimmermann WH, Ferdinandy P, Sluijter JPG. ESC Working Group on Cellular Biology of the Heart: position paper for Cardiovascular Research: tissue engineering strategies combined with cell therapies for cardiac repair in ischaemic heart disease and heart failure. Cardiovasc Res. 2019 Mar 1;115(3):488-500.
(2) Sluijter JPG, Davidson SM, Boulanger, CM, Buzás EI, de Kleijn DPV, Engel FB, Giricz Z, Hausenloy DJ, Kishore R, Lecour S, Leor J, Madonna R, Perrino C, Prunier F, Sahoo S, Schiffelers RM, Schulz R, Van Laake LW, Ytrehus K, Ferdinandy P. Extracellular vesicles in diagnostics and therapy of the ischaemic heart: Position Paper from the Working Group on Cellular Biology of the Heart of the European Society of Cardiology. Cardiovasc Res. 2018 Jan 1;114(1):19-34.
(3) https://www.sluijterlab.com/extracellular-vesicle-inspired-ther
(4) Maring JA, Lodder K, Mol E, Verhage V, Wiesmeijer KC, Dingenouts CKE, Moerkamp AT, Deddens JC, Vader P, Smits, AM, Sluijter JPG, Goumans MJ. Cardiac Progenitor Cell-Derived Extracellular Vesicles Reduce Infarct Size and Associate with Increased Cardiovascular Cell Proliferation. J Cardiovasc Transl Res. 2019 Feb;12(1):5-17.
Please note: this is a commercial profile.