Adam Mence, Senior Brand Manager at L&R Medical UK, discusses the challenges of lower limb wound management and the benefits of driving evidence-based and self-care interventions
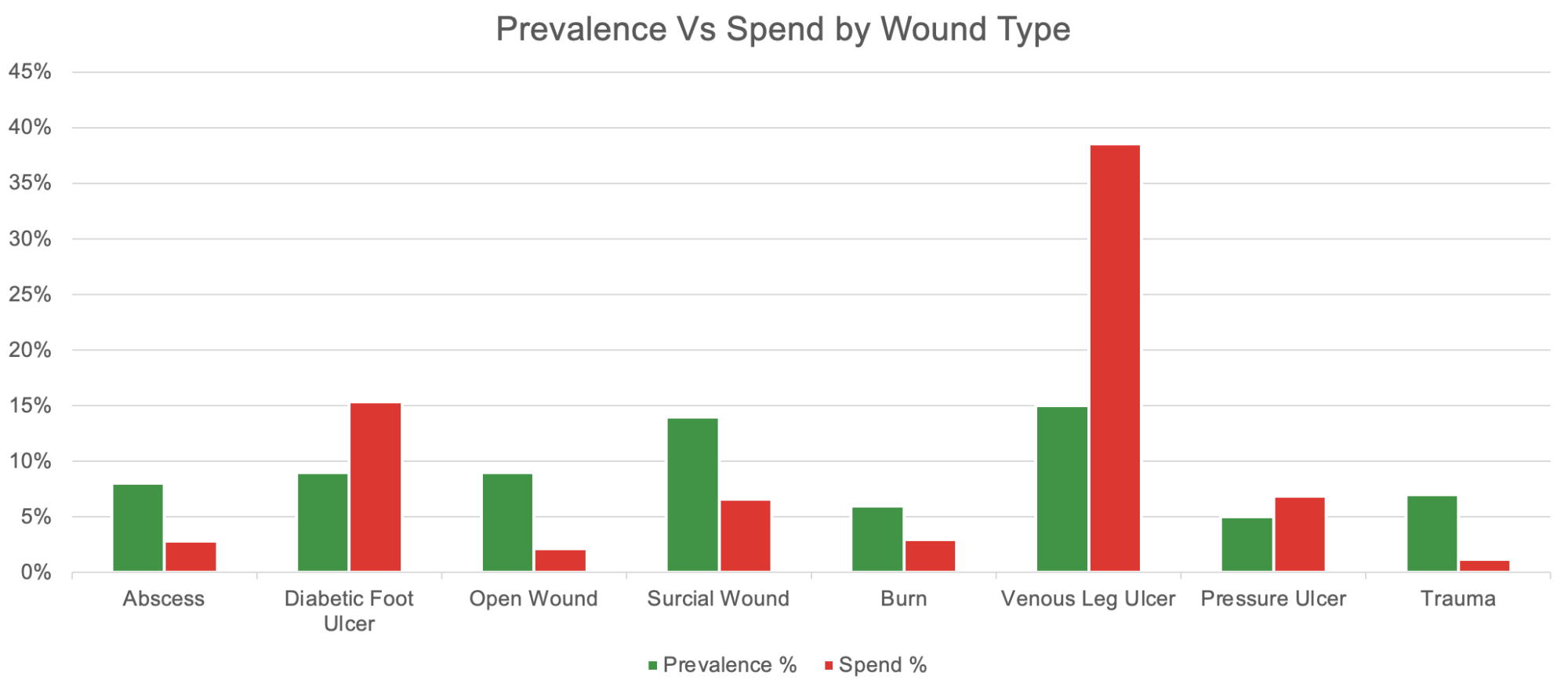
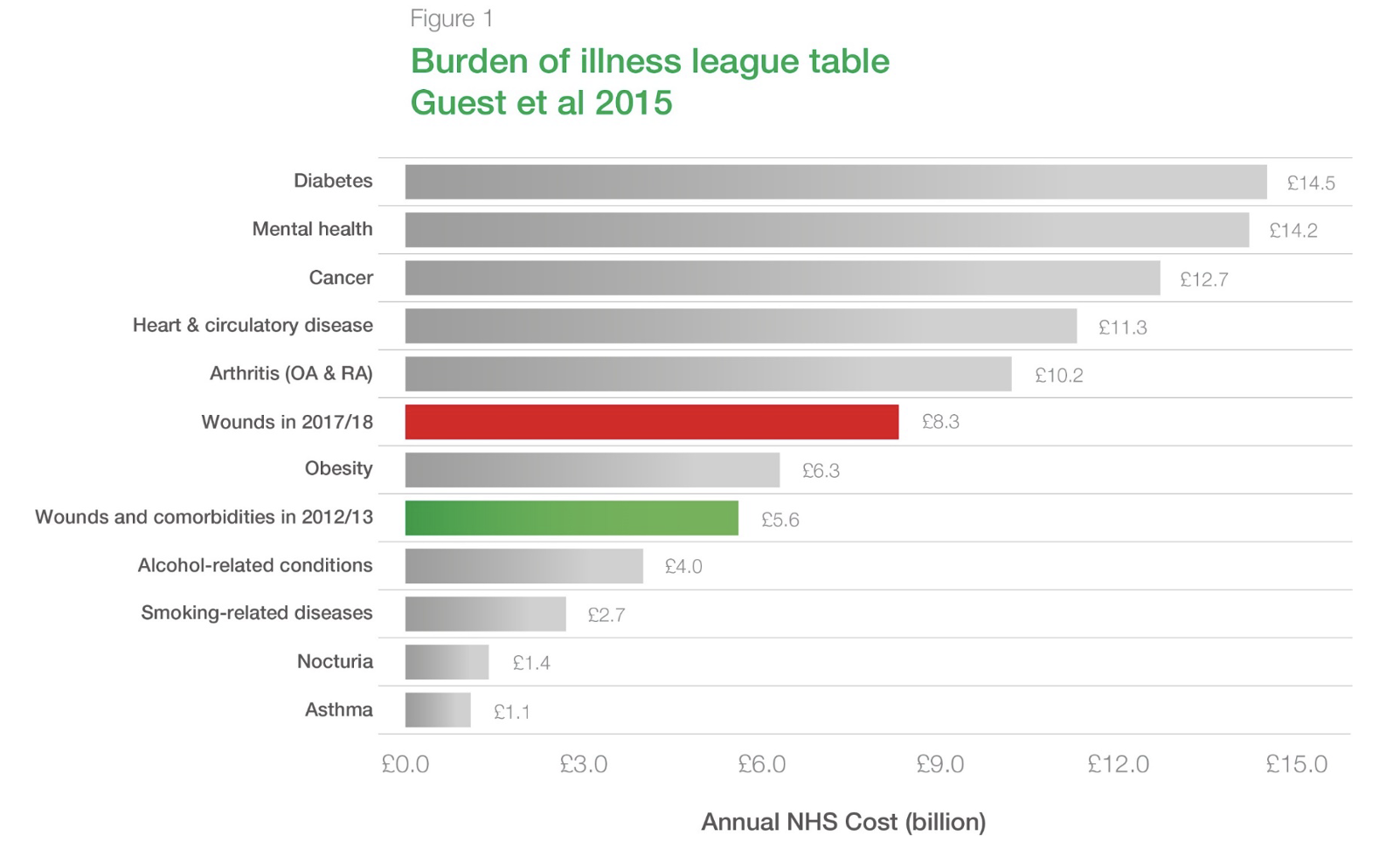
Lower limb ulceration, particularly venous leg ulcers (VLU’s), significantly impacts a patients’ quality of life whilst imposing a substantial financial burden on the National Health Service (NHS). It is estimated that over a million people in the UK are living with lower limb ulceration, costing the NHS over £3.1bn annually. (1) A significant portion of this burden falls on community nursing services, with up to 50% of workload dedicated to chronic wound management. Despite the availability of evidence-based care, the UK’s healing rate for VLU’s remains alarmingly low, at 37% after further compounding the human and financial impact.. (2)
A multifaceted approach is required to transform VLU management in the UK. This approach should focus on implementing evidence-based care, enhancing clinical competency and capability, and empowering patients to engage in self-care.
Implementing evidence-based care
Despite the abundance of evidence and guidance available, there are significant variations in leg ulcer care in practice. Such variations have been highlighted by NHS England’s ‘Betty’s Story’ under the ‘Leading Change, Adding Value’ framework, which provided detailed evidence on unnecessary spending, multiple visits to healthcare providers, extended healing times, and the overall impact on patients’ quality of life.
Health services must strive to eliminate inconsistencies in leg ulcer management, ensuring that all patients receive timely assessments, accurate diagnoses, and treatment plans founded on evidence-based interventions.
Such practice has been demonstrated by the Mid Yorkshire NHS Trust, where an 86% healing rate at 24 weeks has been achieved by standardising care service-wide through the implementation of the Lower Limb Wound Pathway. (3) This pathway includes evidence-based practices such as timely wound assessment, appropriate use of compression therapy, and patient education, leading to an increased uptake of supported self care and improved patient outcomes.
Building competency and capability in the clinical workforce
Although chronic wound management constitutes a significant portion of community nursing workload, there remains a deficiency in concise education provided to nurses both during their initial training and throughout their professional practice.
One of the leading causes of poor healing rates is the underuse of strong compression therapy. (4) Despite the robust, high-level evidence proving its effectiveness in healing VLU, (5, 6) a large proportion of patients are not receiving strong compression. The reasons for suboptimal use of compression are unclear but are likely to be related to a lack of clinical knowledge and confidence surrounding strong compression. (7) New technologies such as adjustable compression wrap systems, provide the simplicity to address low confidence amongst healthcare professionals and enable a broader range of skill mix and roles to deliver effective care, including carers and patients, fostering a shared-care approach. It’s crucial to remember that compression therapy is not just a temporary solution for patients; for many it’s a lifelong commitment. Therefore, treatment plans must prioritise long-term sustainability and effectiveness to ensure ongoing patient management and improve quality of life.
Mid Yorkshire NHS Trust has set up a community-based lower limb wound clinic (staffed by hospital vascular nurses) and implemented a ‘leg ulcer champion’ model across all six networks in the community services (consisting of one to three champions per network). Standardised training on lower limb wound management for the leg ulcer champions was introduced, empowering the community workforce service-wide. Additionally, each leg ulcer champion was provided with the necessary equipment, including Doppler machines to support with assessment, whilst also recognising development opportunities with regular rotation through the vascular nurse-led clinics, direct peer support and access to bespoke online learning.
The resulting impact is not only evident to clinicians but also translates into a noticeable difference in patient experience and outcomes, with community nurses now reporting:
“At first, we were not healing patients; now, by implementing this approach, we can get patients healed within four weeks! Going from dressing ten patients a day to one a week is such a shift in our caseloads.” Our healing rates have doubled, and patients are happier. Patients are getting the treatment they deserve and should have access to.”
Empowering patients to self-care and releasing nursing capacity
Empowering patients is the key to sustainable care within the NHS. Traditional treatment models, often requiring frequent nurse visits, are unsustainable in the face of rising demand and limited resources. Empowering patients to self-care and self-manage is identified as a critical strategy to address this challenge within the NHS Long Term Plan.
Lower Limb Wound Pathway (Atkin and Tickle 2019)
The Lower Limb wound pathway, devised by Joy Tickle and Leanne Atkin (8) was designed to provide a structured, evidence-based approach to assess, treat, and manage patients with wounds on their lower limbs. Its primary purpose is to ensure timely and appropriate care while preventing complications such as infections or chronic non-healing wounds.
Benefits of self-care
- Reduced burden on healthcare professionals: Self-care significantly reduces the number of required nursing visits, freeing up valuable nursing time for patients with complex needs who cannot self-manage. The study by Hallas-Hoyes et al. (2021) found a 90% reduction in healthcare professional contact time with the self-care delivery model. (9)
- Cost savings: Fewer nursing visits and reduced product use translates to substantial cost savings. The study estimated potential savings of £400mn for the UK if 40% of VLU patients adopted self-care (Hallas-Hoyes et al, 2021).
- Improved patient outcomes: Self-care has been linked to improved patient outcomes, including faster healing times, reduced recurrence rates, and increased patient satisfaction. Patients who actively participate in their care often feel more empowered and in control of their health.
- Enhanced sustainability: Self-care can contribute to the NHS’ sustainability goals by reducing travel-related emissions and minimising environmental waste associated with wound care products.
- Empowering patients: Self-care is not merely a cost-saving measure but a fundamental shift towards patient-centred care. It recognises the patient as an active partner in their healing journey, leading to improved outcomes, reduced healthcare burden, and a more sustainable NHS. By embracing self-care, the NHS can provide effective and efficient VLU management while empowering patients to take control of their health.
L&R: Leading the way for sustainable care
L&R Medical UK, a global medical devices company, is committed to supporting the NHS in overcoming the ongoing challenges of wound care and improving patient outcomes. They are passionate about driving evidence-based care and empowering self-care to reduce appointment times and clinical costs and release nursing capacity back to where it’s needed most. L&R Medical UK has developed several initiatives to support these goals, including:
- Standardising care: The implementation of evidence-based care through initiatives like the Lower Limb Wound Pathway. Organisations like Mid Yorkshire NHS Trust have reported healing rates of 86% at 24 weeks by standardising care service-wide. This demonstrates the potential for significant improvement in healing rates through the consistent application of evidence-based practices.
- Self-care delivery model: This model focuses on patient self-care or supported self-care, aiming to reduce the burden on healthcare professionals while maintaining healing rates.
- The dialogue tool: This tool is designed to facilitate better conversations between clinicians and patients, promoting shared decision- making and patient engagement.
- Educational resources: L&R Medical UK provides a range of educational resources for both healthcare professionals and patients, including information on the causes of leg ulceration, treatment options, and self-care techniques.
If you would like more information on how L&R can support your trust with a systematic approach to simplifying lower limb care, please contact us by visiting https://lohmann-rauscher.co.uk/about/contact-us.
References
- Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open. 2020 Dec 22;10(12):e045253. doi: 10.1136/bmjopen-2020-045253. PMID: 33371051; PMCID: PMC7757484
- Gohel MS, Heatley F, Liu X, et al (2018) A randomized trial of early endovenous ablation in venous ulceration. New England Journal of Medicine 378(22): 2105-2114
- Atkin, Leanne and Tickle, Joy (2016) A new pathway for lower limb ulceration. Wounds UK, 12 (2). ISSN 1746-6814
- Cullum N, Buckley H, Dumville J, Hall J, Lamb K, Madden M, Morley R, O’Meara S, Goncalves PS, Soares M, Stubbs N. Wounds research for patient benefit: a 5-year programme of research. Southampton (UK): NIHR Journals Library; 2016 Aug. PMID: 27583319.
- O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev. 2012 Nov 14;11(11): CD000265. Doi: 10.1002/14651858.CD000265.pub3. PMID: 23152202; PMCID: PMC7068175.
- Nelson EA, Adderley U. Venous leg ulcers. BMJ Clin Evid. 2016 Jan 15;2016:1902. PMID: 26771825; PMCID: PMC4714578.
- Adderley UJ, Thompson C. Confidence and clinical judgement in community nurses managing venous leg ulceration – A judgement analysis. J Tissue Viability. 2017 Nov;26(4):271-276. doi: 10.1016/j. jtv.2017.07.003. Epub 2017 Jul 19. PMID: 28747258.
- Atkin L, Tickle J (2019) A new pathway for lower limb ulceration. Wounds UK 12(2): 32–6
- Hallas-Hoyes L, Williamson S, Kerr A, Andrews T, Calladine L. An advanced self-care delivery model for leg ulcer management: a service evaluation. J Wound Care. 2021 Sep 2;30(9):751-762. doi: 10.12968/ jowc.2021.30.9.751. PMID: 34554835.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.