Barak Katz, VP and GM Essence SmartCare, discusses the future of fall prevention and establishing more proactive elderly care, post COVID-19
While the COVID pandemic has been exceptionally challenging for the NHS and other care agencies, there are emerging knock-on effects that will likely result in further challenges. Beyond the reported postponed appointments and surgeries, one area that is being overlooked is the increased risk of unreported falls for the elderly.
Given the need for social distancing and reduced access to health and other vital services, high-risk individuals have had to live more independently, through prolonged periods of isolation. Now more than ever, they are at risk of preventable trips and falls, and are less likely to report these incidents. In fact, The National Falls Prevention Coordination Group (NFPCG) – the leading body for prevention of falls and care of fall-related injuries in England – highlighted the gravity of the situation in a recent report, urging care teams to address the issue before it gets out of hand.(1)
The lack of clarity regarding trips and falls has been discussed for quite some time. There are around 255,000 fall-related emergency hospital admissions in England among patients each year, with around 5% of cases resulting in fracture and hospitalisation; collectively costing the NHS over £2.3 billion per annum.(2)
Risk of falls
Addressing the risk of falls should be a top priority, especially at this difficult time when many elderly people are living alone or isolating. However, as our own research revealed, around 75% of all falls still go unreported. If individuals are not reaching out and raising the subject with their families or carers, and care teams do not have the solutions in place to record and prevent such incidents, how can the sector mitigate the risk of falls?
More visibility into what is actually going on is needed. As the UK COVID ‘Track and Trace’ system has proven, the ability to record and establish accurate datasets are key to tackling some of societies biggest healthcare challenges. With regards to elderly or social care, teams require insight into the events that led up to the fall. However, there are simply too many gaps in the data.
Technology
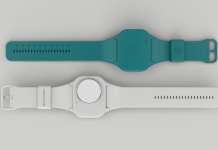
Whilst there have been some recent technological developments such as smart sensors and other telecare solutions, most current fall detectors are based on accelerometer technology, which only detects certain types of incidents, and at times, records accidents in error. Despite these devices tracking an elderly patients’ movements, most falls simply go unrecorded or are reported inaccurately.
This represents a serious challenge, particularly if the more serious falls that result in injury are not being reported. As our research suggests, less than half of those in residential care actually wear fall detection devices as they find them too invasive, meaning care teams cannot record the events leading up to a serious incident, and so preventative measures simply cannot be put in place. More proactive social care is needed to record, prevent, and manage falls.
To truly limit the risk of injury or serious trauma, an entire appraisal of the fall sufferer’s situation is needed. After all, prevention is not possible without anticipation. More information needs to be recorded and shared, with the more effective telecare solutions reporting on the circumstances leading up to the incident so care teams can retrace their steps. Relying on legacy systems that confirm whether a fall indeed took place and call for help, is simply no longer viable.
Culture change in care
There should be a culture change in care, where elderly individuals feel more comfortable discussing their fall incidents, with less overt judgement being made about their behaviours. Even now, seven in ten falls rely on the individual recounting the events leading to the fall themselves, rather than having actual data about what happened to occasion the fall.
A new way is therefore needed, a form of non-linear fall prevention, that deploys modern telecare technology that provide care teams with a bigger, richer picture. This new approach, using multiple unobtrusive sensors, allows care teams to monitor an individual’s movement throughout the household, with machine learning analysing trends, patterns of behaviour and tracking anomalies, such as more frequent bathroom visits, periods of long seated rest, or fewer trips to the kitchen.
Only by improving the accuracy of recorded falls from end to end, and drawing upon incident logs and previous case history, can care teams gain real insight into what led to the fall and put preventative measures in place. Whether the solution is installation of grab rails, improved flooring, or lighting, or even reconsidering the resident’s current home setting, only by identifying all risk factors for that individual, can teams make widespread changes and offer more personalised care programmes that will allow people to remain independent for longer with continued decent quality of life.