Professor Peter J. Houghton from the Greehey Children’s Cancer Research Institute discusses new approaches to pediatric cancer treatment specifically for BRAF-mutant pediatric glioma
Low-grade glioma (LGG) is the most frequently diagnosed brain tumor in children, and although five and ten-year survival is quite high, this does not reveal the toxicity of current therapies. Conventional treatment includes intensive chemo-radiation therapy that can lead to cognitive decline, malignant transformation, and other life-debilitating or -threatening sequelae. (1) The 15-year incidence of adverse outcomes such as blindness, hearing loss, obesity, and hormonal imbalance is 18%, 22%, 53%, and approximately 25%, respectively. Among survivors assessed for intellectual function, 34% had an intelligence quotient (IQ) below average. Treatment-resistant progressive disease is the most common cause of death. (2)
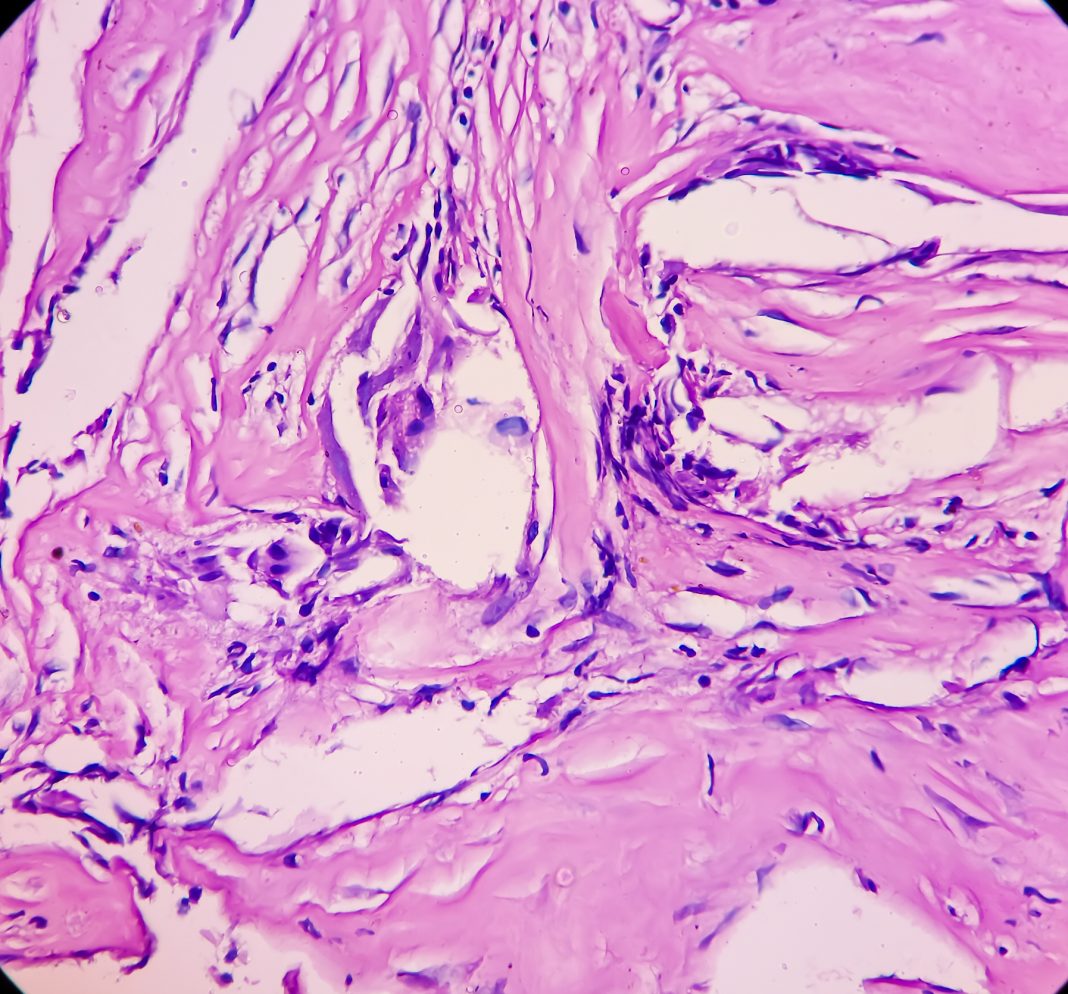
KIAA1549-BRAF fusion
Genomic studies have shown that in low-grade tumors (LGG or juvenile pilocytic astrocytoma), ~80% have a tandem duplication involving the KIAA1549 and BRAF genes that generate constitutively active fusions. (3) These fusions activate BRAF and downstream signaling, leading to cellular proliferation. In both phase 1 and phase 2 trials of selumetinib – an inhibitor of MEK downstream of BRAF – patients with tumors harboring the KIAA1549-BRAF fusion had good outcomes with most having tumor regression and remaining on treatment for 24 months, the duration of the phase 2 study. (4)
In the order of 20% of LGG have activating point mutations of BRAF, most frequently the V600E variant. Such activating mutations are identified in diffuse astrocytomas (23%), gangliogliomas (33%), and pleomorphic xanthoastrocytoma (70%). Some 10-15% of pediatric glioblastomas and many epithelioid glioblastomas also carry this mutation. Drawing from available databases (ACS and CBTRUS), approximately 1400 new pediatric BRAF mutant brain tumors are diagnosed in the US annually.
In the selumetinib phase 2 trial, these patients had inferior outcomes compared to patients with tumors driven by the KIAA1549-BRAF fusion, indicating a higher risk and the need to develop more effective therapeutic approaches. In the Lancet Oncology editorial, Bouffet (5) emphasized that a majority of BRAF(V600) mutant tumors either progress on treatment (i.e., become resistant) or progress rapidly when selumetinib is terminated and stressed the importance of further studies with chemotherapy or other agents to prevent the high relapse rates with selumetinib. One such approach is vertical targeting of the MAPK signaling pathway. Unlike models driven by KIAA1549-BRAF fusions, those with BRAFV600E are sensitive to direct inhibitors of BRAF.
Thus, inhibiting BRAF and MEK in the MAPK pathway makes sense and has been shown to be more effective thansingle agents targeting BRAF or MEK in treating advanced melanoma driven by the V600 mutant BRAF in adults. In adult patients with melanoma, adding the BRAF inhibitor dabrafenib to trametinib (MEK inhibitor) increased progression-free survival (PFS) from 5.8 to 9.4 months (6), suggesting that vertical targeting of MAPK was more effective and possibly suppressed the emergence of resistance.
Combination treatment
Several small studies have indicated that BRAF inhibitors can cause tumor regression in V600 mutant glioma, and selumetinib caused responses in both phase 1 and phase 2 trials, although some were transient. Thus, based on the efficacy of trametinib combined with dabrafenib in melanoma, investigating these agents in V600 mutant LGG was appropriate, if not particularly innovative.
In a pediatric clinical trial reported recently (clinical trials.gov identifier NCT02124772), the tolerability and efficacy of trametinib alone or in combination with dabrafenib was investigated in relapsed patients. (7) The results of this complex study are of interest and importance. Firstly, the combination was tolerated better than trametinib alone, with only 22% of patients treated with combination treatment discontinuing treatment for toxicity compared to 54% in the trametinib alone cohort (although the number of patients in this part of the study was small). Secondly, the objective response rate for the combination treatment was 25% (95% CI, 12.1 to 42.2) compared to 15% (95% CI, 1.9 to 45.4) for trametinib alone.
Perhaps of greater significance was that the progression-free survival in the drug combination cohort was double that in the trametinib alone cohort (36.9 months versus 16.4 months). Thus, combination treatment compares favorably with single-agent trametinib. However, these data do not inform whether combination treatment is superior to dabrafenib alone. Further randomized clinical trials will be required to determine the answer. However, as first-line therapy combination treatment with trametinib/dabrafenib was clearly superior to chemotherapy in a randomized clinical trial and will be the new standard of care for these patients.(8)
The future challenge is to develop more efficacious and potentially curative therapy for BRAF V600 mutant disease. Data from preclinical patient-derived xenograft (PDX) glioma models with this BRAF mutation shows that many mechanisms may mediate acquired resistance to trametinib, similar to data for clinically acquired resistance to trametinib in melanoma. The combination of trametinib with rapamycin prevents or delays the emergence of resistance independent of the mechanism of resistance to trametinib. (9) However, combining MEK inhibitors with rapamycin analogs that inhibit mTOR has proven difficult in a clinical setting due to toxicity. Of interest, rapamycin appears to retard the emergence of resistance to X-radiation therapy in these preclinical PDX models. However, further work is needed to confirm the value of this approach.
Although the mechanism for rapamycin action is not yet elucidated, X-radiation induces cells into senescence, and potentially, some of these cells recover to repopulate the tumor. Rapamycin appears to kill senescent cells, which may account for the delay or prevention of the emergence of radiation resistance in these models. The effects of X-radiation are cytotoxic (i.e., kills tumor cells) thus, the effect of rapamycin appears to enhance cell killing or kill cells that would repopulate the tumor bed following radiation. Whether combining rapamycin analogs with focused X-radiation will be as toxic as combining MEK and mTOR inhibition remains to be determined. The challenge remains how to eradicate BRAF V600-mutant disease.
References
- Merchant TE, et al. Pediatric blood & cancer 2013;60:1037-43.
- Upadhyaya SA et al. Pediatric blood & cancer 2018. 65(1):10.1002/pbc.
- Pfister S, et al. J Clin Invest 2008;118:1739-49.
- Fangusaro J et al. Lancet Oncol 2019;20:1011-22.
- Bouffet E. Lancet Oncol 2019;20:900-1.
- Flaherty KT et al. N Engl J Med 2012;367:1694-703.
- Bouffet E et al.,J. Clin Oncol 2023; 44: 664-675.
- Bouffet E et al., N Engl J Med 2023;389:1108-1120.
- Li F et al. Clin Cancer res. 2022; 28:3836-3849

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.