Here, Doctor Peter J Houghton explains current therapies for childhood brain cancer what needs to change to ensure better outcomes for children diagnosed with astrocytoma in the future
Cancer in children is rare, representing less than 1% of all cancers in the U.S. Yet, despite major advances in treating childhood cancer, it remains the major cause of disease-related death in children up to 19 years of age in the U.S. It is estimated that 1 in 285 children will be diagnosed with cancer.
Brain cancer and children
Hematologic malignancies (leukemia and lymphoma) represent the most frequently diagnosed cancers, with brain tumors being the most common solid tumors of childhood. Brain tumors appear to be more prevalent in white children (82.6%) and in males (53.2%). It is this area of childhood cancer that molecular genetics have made great advances in understanding the molecular mechanisms associated with each type of brain cancer, yet more children die from brain tumors than any other childhood cancer.
Genomics studies of medulloblastoma, a malignancy of the cerebellum (hind brain) have shown that what was considered to be a single entity is now understood to be at least four entities differing in the cell of origin and response to chemotherapy. Expression profiling suggests that ependymoma may comprise nine subtypes. The anticipation from such studies is that such genetic information will lead to effective and less toxic therapies.
The World Health Organization (WHO) categorized astrocytomas as ‘diffuse astrocytoma’ that includes Grade II and III diffuse astrocytoma, Grade IV glioblastoma and diffuse gliomas of childhood, or ‘other astrocytic tumors’. The latter group includes pilocytic astrocytoma, pleomorphic xanthoastrocytoma, anaplastic pleomorphic xanthoastrocytoma and subependymal giant cell astrocytoma.
Understanding astrocytoma
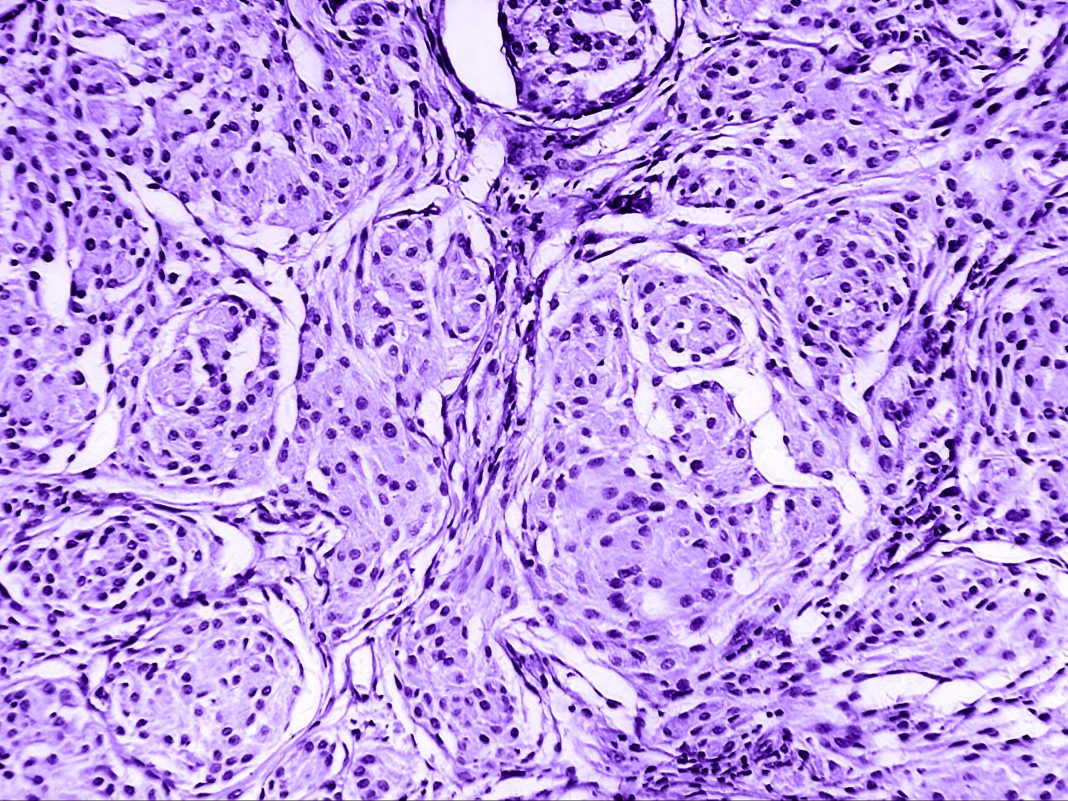
The most common brain tumor in children is astrocytoma. These tumors can occur in any part of the brain, and are derived from astrocytes, a type of glial cell that provides nutrition to neurons in the brain. Astrocytoma may occur as a familial cancer or as a sporadic cancer.
There is an increased risk of low-grade astrocytoma with a genetic condition called neurofibromatosis 1 (NF1). These familial astrocytoma’s are associated with mutations in the NF1 gene that encodes a negative regulator of RAS, leading to constitutive signaling through the MAP kinase and PI3 kinase pathways, and continued cell proliferation. Sporadic low-grade astrocytoma, often referred to as Juvenile Pilocytic Astrocytoma (JPA), is also associated with activation of the MAP kinase signaling pathway. These tumors are indolent (slow growing) and well circumscribed without invasion into surrounding brain tissue.
What have continued genetic studies on these tumors shown us?
Genomic studies have shown that ~90% of these low-grade tumors have a tandem duplication involving the KIAA1549 and BRAF genes that generate constitutively active KIAA1549::BRAF fusions(1). Higher grade tumors tend to have activating point mutations of BRAF(2), most frequently the V600E variant. Such activating mutations are identified in diffuse astrocytomas (23%), gangliogliomas (33%), and pleomorphic xanthoastrocytoma (70%). Some 10- 15% of pediatric glioblastomas and many epithelioid glioblastomas also carry this mutation. Drawing from available databases (ACS and CBTRUS) approximately 1400 new pediatric BRAF mutant brain tumors are diagnosed annually, also 350 adult brain tumors(3).
Outcome for children diagnosed with astrocytoma is determined by stage, and site in the brain. For pilocytic astrocytoma (Grade I, also referred to as low-grade glioma) 5-year survival is ~95% following surgery as the primary treatment. For Diffuse astrocytoma (Grade II) survival falls to 80-85%, whereas for Grade III (anaplastic astrocytoma), glioblastoma multiforme (Grade IV), and diffuse intrinsic pontine glioma 5-year survival is only 25%, 20%, and 2% respectively.
Current treatments and chemo-radiation therapies
Treatment for Grade I (benign) tumors is largely restricted to surgery and complete resection results in cures for most patients where tumor is surgically accessible. For patients with incomplete tumor resection a second surgery remains the primary treatment. Complete resection is achieved in over 90% of Grade I tumors in the cerebellum. However, for those patients where complete resection is not possible chemotherapy is used with curative intent.
Current treatment includes intensive chemo-radiation therapy that includes carboplatin-vincristine or 6-thioguanine-procarbazine-CCNU and vincristine. Radiation doses vary between 45-54Gy. Such chemo-radiation protocols can lead to cognitive decline, malignant transformation, and other life- debilitating or -threatening sequelae(4). Thus, while the 5- and 10-year overall survival statistics look impressive, the 15-year incidence of adverse outcomes such as blindness, hearing loss, obesity, hormonal imbalance was 18%, 22%, 53% and approximately 25%, respectively(5). Among survivors assessed for intellectual function, 34% had an intelligence quotient (IQ) below average. Treatment-resistant progressive disease is the most common cause of death(6). Because of the sequelae, radiation is not used routinely, especially in young children.

Diffuse astrocytoma and poorly defined margins
Diffuse astrocytoma (Grade II) is referred to as a non-malignant low- grade tumor and is characterized by poorly defined margins with clusters of tumor cells invading surrounding normal brain tissue. Tumors tend to arise in the cerebral hemispheres. Although mutations in the isocitrate dehydrogenase (IDH1) gene are more common in acute myeloid leukemia (25%), such mutations are found in Grade II astrocytoma, and these tumors tend to respond better to treatment and patients have a better prognosis. However, diffuse astrocytoma’s can recur after surgery (primary treatment) and can transform to higher grade malignancies.
For older children, secondary treatment for incomplete resection is ionizing radiation or more recently, proton beam therapy available at some centers. For younger patients, where radiation treatment is avoided during brain development, chemotherapeutics such as temozolomide may be used. The median survival for patients with Grade II tumors is 8 years, but 40% of patients survive over 10 years.
The rarity of Grade III and IV
Grade III and IV gliomas (high-grade, HGG) are relatively rare in children, constituting approximately 7.9 and 9.0% of diagnoses, respectively in children up to the age of 20. Differences between adult and childhood HGG suggest that the mechanism(s) of glioblastomagenesis may be different between these populations(7). For example, amplification or overexpression of the epidermal growth factor receptor (EGFR; ERBB1) found in 30-50% of adult HGG is relatively rare in pediatric HGG and similarly mutations in the PTEN gene, that encodes a negative regulator of the phosphoinositide 3’ kinase (PI3K) pathway are rare in childhood HGG whereas mutations occur in 50% of adult HGG.
However, activation of Akt is found in many (79%) of childhood HGG and is associated with poorer prognosis(8). Five-year survival for Grade III and IV gliomas remains grim. Standard treatments include radiation up to 54Gy and temozolomide, a DNA methylating agent that induces modification on O6-guanine as the cytotoxic lesion. Tumors that lack the DNA repair enzyme methylguanine DNA methyltransferase (MGMT), due to promoter methylation that causes gene silencing, are more sensitive to temozolomide and chloroethylating nitrosurea drugs such as carmustine. However, the frequency of MGMT- deficient childhood HGG is far lower than in adult tumors thus rendering temozolomide or carmustine essentially ineffective in most tumors replete for MGMT.
Diffuse intrinsic pontine gliomas
Diffuse intrinsic pontine glioma (DIPG), a highly aggressive brain stem malignancy, appears genetically distinct in that the oncogenic driver is in chromatin remodeling genes histone H3A (H3F3A) and histone H3b (HIST1H3B), encoding histone H3 variants H3.3 and H3.1, respectively. H3.3 mutations occur at lysine 27 or glycine 34 with methionine replacing lysine and valine or arginine replacing glycine (K27M or G34V/R). Missense mutations occur in up to 80% of childhood DIPG but is rare in adult HGG. Prognosis for patients with DIPG is particularly poor, as diffuse infiltration of the surrounding brain stem precludes surgery.
There is limited response to current therapies, and focused high-dose radiation is the only effective palliative treatment causing temporary tumor shrinkage that may last 6-9 months. Experimental approaches such as convection-enhanced delivery that potentially circumvents the blood-brain barrier have been explored using antibody-radionuclides 124I-8H9. Because the prognosis for DIPG is so poor many new drugs are being tested in patients early in their disease, including immuno-therapeutics such as chimeric antigen T cell receptor (CAR T) cells targeting the ganglioside GD2 that is delivered intracerebroventricularly. However, because of the potential toxicity to normal GD2-expressing brain tissue, this therapy has to be administered with intensive supportive care.
As discussed earlier, a common characteristic of most gliomas is the activation of the MAP kinase pathway and trials in adults had established the value of MAPK inhibitors for the treatment of BRAF-mutant melanoma. Activation of MAPK in childhood glioma can be a consequence of NF1 mutation, the KIAA1549::BRAF fusion or activating point mutations in BRAF, such as V600E. As Grade I, -II gliomas are benign, it has been impossible to generate cell lines or patient-derived xenografts (PDX) in mice.
However, cell lines and PDX Grade 3 models can be established. Importantly for development of drugs targeting the MAPK pathway, it was shown that a murine fibroblast cell line engineered to express the KIAA1549::BRAF fusion was sensitive to MEK inhibitors but not to early generation BRAF inhibitors, further, studies by the Pediatric Preclinical Testing Program (PPTP) showed that the MEK inhibitor, selumetinib, was active only in a BRAFV600E mutant anaplastic astrocytoma, not in a similar astrocytoma with wild type BRAF, or in approximately 50 other pediatric cancer models in mice. These data, in part, stimulated Phase I testing of selumetinib in low-grade glioma and subsequent Phase II evaluation in NF1 and BRAF-mutant patient cohorts with recurrent, refractory or progressive disease (9). Selumetinib induced similar responses in NF1 and BRAF-mutant cohorts (40% vs 36%), but importantly patients with KIAA1549::BRAF fusions had prolonged tumor control, whereas those with BRAFV600E mutations either failed on treatment, or relapsed at the end of two years (the duration of treatment for the trial) when drug dose was reduced or therapy stopped.
Is replacing chemo-radiation with selumetinib a reality?
The conclusion from this study was that selumetinib could replace standard chemo-radiation, and a trial to compare outcomes is ongoing. Also clear from the study is that inhibition of MEK provides effective control for most tumors but is not curative. Bouffet (10) in an editorial emphasized that a majority of BRAF(V600E) mutant tumors either progress on treatment (i.e. become resistant), or progress rapidly when selumetinib is terminated, and stressed the importance of further studies with chemotherapy or other agents such as mTOR inhibitors to prevent the high relapse rates with selumetinib. Recent studies of BRAF(V600E) mutant glioma PDX models strongly suggest that drugs that inhibit MAPK signaling also inactivate mTOR complex 1 (TORC1) and that dual inhibition of MAPK and TORC1 is required for tumor regression(11).
In contrast, in several Grade IV adult glioblastoma models that are less sensitive to treatment, inhibition of MEK induces Akt activation and maintenance of TORC1 signaling with continued tumor growth. As with the clinical situation, PDX models of BRAF(V600E) glioma in mice initially respond to treatment but become resistant after 18-24 weeks of treatment with trametinib, a potent MEK inhibitor. While the mechanisms for acquired resistance are multiple in these models, as with BRAF(V600E melanoma), one important observation was that combining trametinib with low dose intermittent treatment rapamycin (a specific inhibitor of TORC1) either prevented or significantly retarded the emergence of resistance.
Searching for better outcomes for children diagnosed with astrocytoma
Brain tumors in children remain a predominant cause of death where complete surgical resection is not achieved, and for those children, traditional chemo-radiation treatments may lead to unacceptable sequelae. While high-grade astrocytoma/glioma remains a clinical challenge, the finding that many astrocytic tumors are ‘driven’ by activating alterations in the MAPK signaling pathway has re-focused therapies to incorporate single or multiple drugs that inhibit sequential steps in the pathway, such as combining MEK and pan-RAF inhibitors providing effective and less toxic alternatives to traditional therapeutic strategies.
Understanding the oncogenic drivers and mechanisms of acquired drug resistance will undoubtedly contribute to more effective treatments and better outcomes for children diagnosed with astrocytoma in the future.
References
- S. Pfister et al., J Clin Invest 118, 1739-1749 (2008).
- K. C. Schreck, S. A. Grossman, C. A. Pratilas, Cancers (Basel) 11, (2019).
- Q. T. Ostrom et al., Neuro Oncol 21, v1-v100 (2019).
- T. E. Merchant et al., Pediatric blood & cancer 60, 1037- 1043 (2013).
- P. de Blank, P et al., Curr Opin Pediatr 31, 21-27 (2019).
- S. A. Upadhyaya et al., Pediatric blood & cancer 65, (2018).
- B. S. Paugh et al., J Clin Oncol 28, 3061-3068 (2010).
- D. Rizzo et al., Biomed Res Int 2015, 215135 (2015).
- J. Fangusaro et al., Lancet Oncol 20, 1011-1022 (2019).
- E. Bouffet. Lancet Oncol 20, 900-901 (2019).
- F. Li et al., Clin Cancer Res 28, 3836-3849 (2022).
Grant Support: R01CA258381 and U01CA263981 from the National Cancer Institute and RP160716 from the Cancer Prevention and Research Institute of Texas (CPRIT)

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.