Dr Peter J Houghton from Greehey Children’s Cancer Research Institute discusses the obstacles in developing new treatments for childhood cancers and new approaches in preclinical testing
In my previous article for Open Access Government, I focused on the challenges of developing novel therapies for children with glioma, the most prevalent brain cancer in children. Here, I want to discuss the challenges at the preclinical stage of drug development, an area of research that will be altered significantly by the Research to Accelerate Cures and Equity for Children Act (RACE for Children Act).
This U.S. law requires the Food and Drug Agency (FDA) to develop a list of molecular targets and molecular targets of new drugs and biologics in development that are determined to be relevant to pediatric cancers. The objective is to facilitate a more rapid introduction of new drugs into the pediatric cancer armamentarium. The FDA may now require pediatric assessments when molecular targets under FDA review are considered relevant to childhood cancer.
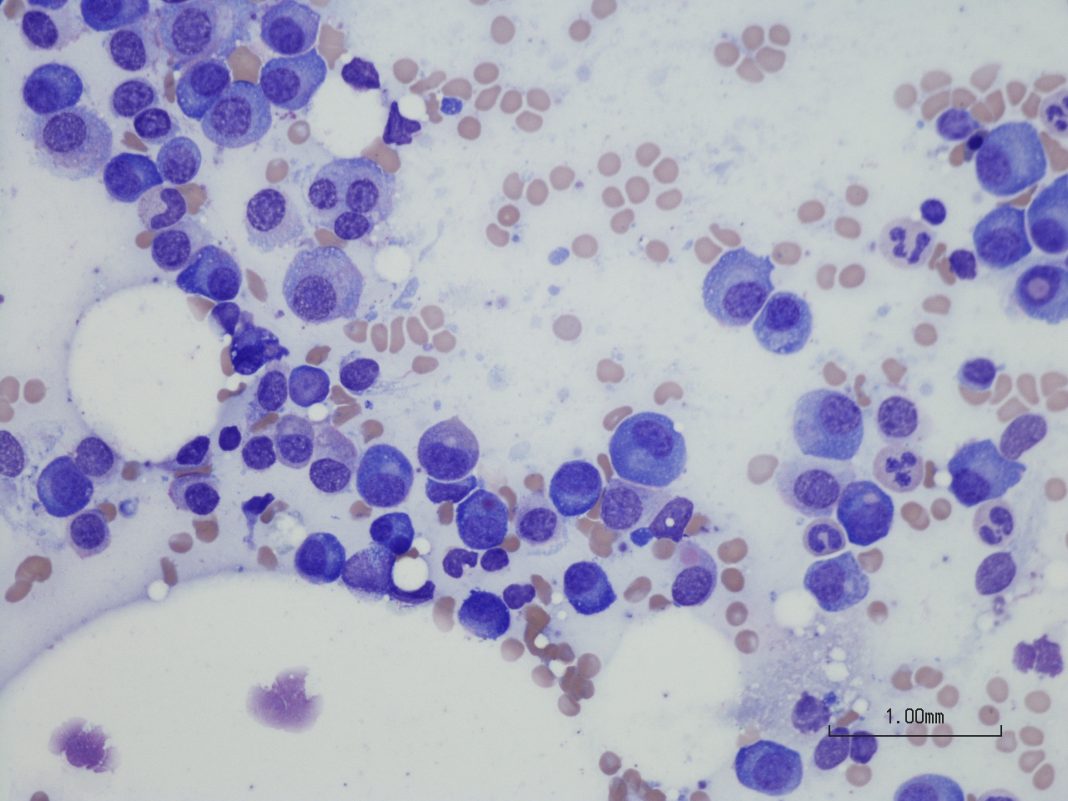
The diversity of childhood cancers
In the last two decades, genetic studies have revealed the complexity of childhood cancers that were once considered homogeneous entities. For example, medulloblastoma, a tumor of the hindbrain, can now be stratified into four separate genetic entities with potentially different molecular targets. Ependymoma, another brain tumor, may have eight molecular subtypes.
Similarly, non-brain solid tumors can be sub-grouped according to either genomic aberrations (mutations or gene fusions) or gene expression profiles. Based on genomic studies, leukemias, which comprise approximately half of childhood cancer, can be classified into 17 groups. This molecular diversity poses enormous challenges to developing novel molecularly targeted drugs or biologics.
In the U.S., approximately 200 cases of medulloblastoma are diagnosed annually; thus, the number of patients eligible to receive a targeted drug, assuming equal distribution of molecular subtypes, is diminishingly small.
From a preclinical perspective developing targeted therapies for multiple molecular subtypes also presents challenges. We know from adult clinical studies that targeting a molecular driver, such as mutant BRAF in melanoma and colon carcinoma, can have very different outcomes.
For BRAF-driven melanoma, response rates for BRAF or MEK inhibitors are high, and these agents have radically improved outcomes. In contrast, the same drugs in the context of colon cancer have had a very modest effect. Thus, despite a common molecular driver, context appears critical in determining outcome.
Consequently, because a molecularly targeted drug is active against an adult cancer does not necessarily mean it could have activity against a childhood cancer with the same molecular defect.
Testing molecularly targeted drugs and biologics
How, at a preclinical level of development, can drugs or biologics with specific molecular targets be evaluated as required under the RACE Act? Potentially, one could genetically engineer the molecular aberration into the appropriate tissue of a mouse (Genetically Engineered Mouse Models or GEMMS).
However, this is expensive and time-consuming hence not on the radar screen for pharmaceutical companies. An alternative is developing patient-derived xenografts (PDXs), where tumor tissue is directly transferred to an immune-deficient mouse. Establishing PDX models is also very expensive and time-consuming but has been the focus of academic groups in the U.S. and Europe.
There are probably over 1000 models of pediatric cancers established in mice, and most have genomic characterization, thus providing a resource for testing molecularly targeted drugs or biologics. However, it is important to be aware that there can be clonal evolution or clonal selection during the process of engraftment in mice. Consequently, direct comparison between the drug response for a PDX may not be the same as in the donor patient.
Therefore, the value of ‘co-clinical trials’ where the response of the PDX to different drugs is used to predict or even direct subsequent therapy in the donor patient must be viewed with caution.
In many instances, knowledge of the genetic driver does predict the success of drugs that target the oncogenic ‘driver’ or downstream signaling pathways activated by the driver mutation. Good examples are MEK inhibitors in children with BRAF-mutant low-grade glioma.
However, the response in patients with higher-grade diffuse anaplastic astrocytoma, or glioblastoma, can be transient or no response despite the same underlying genetic change. So, with knowledge of the genomic diversity of a cancer type (even those with the same driver aberration), the complexity of estimating the value of a new drug increases and leads us to reconsider how preclinical testing is designed.
Traditionally, relatively large groups of PDX-bearing mice (8-10 per group) have been used to assess the growth of drug-treated tumors compared to tumors in untreated mice. While this design allows the statistical significance of a drug effect, it limits the number of PDX models that can be assessed.
Further, statistical significance does not mean biologically meaningful antitumor activity. For example, the drug may slow tumor growth by 10-20% to show ‘statistically significant’ activity at a P=0.05 level, whereas to be considered active in a pediatric cancer clinical trial, tumor shrinkage (regression) has to be observed. For accurate translation of preclinical data, closer alignment of activity endpoints is required.
An alternative approach to preclinical testing
An alternative approach was developed initially at Novartis,(1) where thirty melanoma xenograft models were used to simulate a ‘clinical trial,’ using only one mouse per tumor line as a control (untreated) and one mouse that received treatment. Also, a retrospective of over 2000 drug-tumor studies by the NCI-supported Pediatric Preclinical Testing Program (PPTP) that used 8-10 mice per treatment group showed that a single mouse per treatment could accurately predict the group median response in approximately 80% of studies, and accurately predicted the objective response rate for the 83 xenograft models for 66 of 67 drugs tested. (2)
The importance of these studies is that this ‘single mouse’ experimental design allows assessing a drug against a large number of models with similar molecular characteristics or genetic drivers and offers an opportunity to determine mechanisms that may confer resistance to the agent, and hence identify potential biomarkers of tumor response. Single-mouse testing is now incorporated into the major pediatric preclinical testing approaches in the U.S. and Europe.
References
- Gao H et al Nature Med, 2015
- Murphy B et al Cancer Res, 2016

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.