Mark Rutherford, Associate Professor at Washington University School of Medicine, discusses the burden and causes of hearing dysfunction, as well as the possible solutions for mitigating glutamate excitotoxicity
The cochlea, the snail-shaped organ of the inner ear located deep in the skull, contains approximately 15,000 sound receptors called sensory ‘hair cells’ and approximately 50,000 nerve fibers sending sound information to the brain. Although that may seem like a lot, it is not compared to the approximately 100 billion neurons in the brain. These hair cells and nerve fibers are all we get for life, and they are gradually lost over time due to aging. Unfortunately, environmental factors accelerate cochlear decline over time. One of those environmental factors is loud sounds.
Today, we live in an environment of sound at levels that far exceed those under which our species evolved, especially those of us with noisy occupations or recreational activities. For example, military personnel are particularly vulnerable to hearing loss, making hearing disorders (including tinnitus) the number one disability claim of the U.S. Veterans Administration.
Auditory dysfunction through acoustic trauma
One of the leading causes of hearing loss and auditory dysfunction is acoustic trauma, which can occur from exposure to very loud sounds, causing the destruction of our precious cochlear hair cells. Also, prolonged periods of moderately loud sounds that may not kill the hair cells themselves nonetheless destroy the cochlear synapses – the physical connections between hair cells and nerve fibers.
Some may be lost forever once these connections are broken, leading to auditory dysfunction, such as difficulty hearing speech in the presence of background noise. These hearing-in-noise difficulties often manifest in people with normal audiograms, which test a person’s ability to hear soft tones in quiet. This phenomenon gave rise to the term ‘hidden hearing loss’ because such hearing disorders are not reflected in the audiogram. This form of hearing dysfunction is particularly insidious because it can happen slowly over time due to prolonged exposure to sounds that are only moderately loud.
Hearing disorders can lead to communication difficulties and social isolation, which are associated with an increased likelihood of developing dementia in later life. A 2020 commission report by the Lancet lists hearing loss as one of the top risk factors for dementia.
Without effective therapies to restore normal hearing through cellular regeneration, hearing loss is permanent and only partly treatable with hearing aids and cochlear implants. Physical protection (ear plugs and earmuffs) can be effective when used appropriately under controlled conditions. However, using physical protection in real-world situations is often suboptimal due to inconvenience, discomfort, poor fitting, or intentional non-compliance because they hinder hearing. Earplugs and earmuffs may reduce situational awareness, which can be life-threatening. The fragility of hearing and our inability to fully restore it underscores the need to prevent such permanent damage from occurring in the first place.
Noise-induced hearing disorders
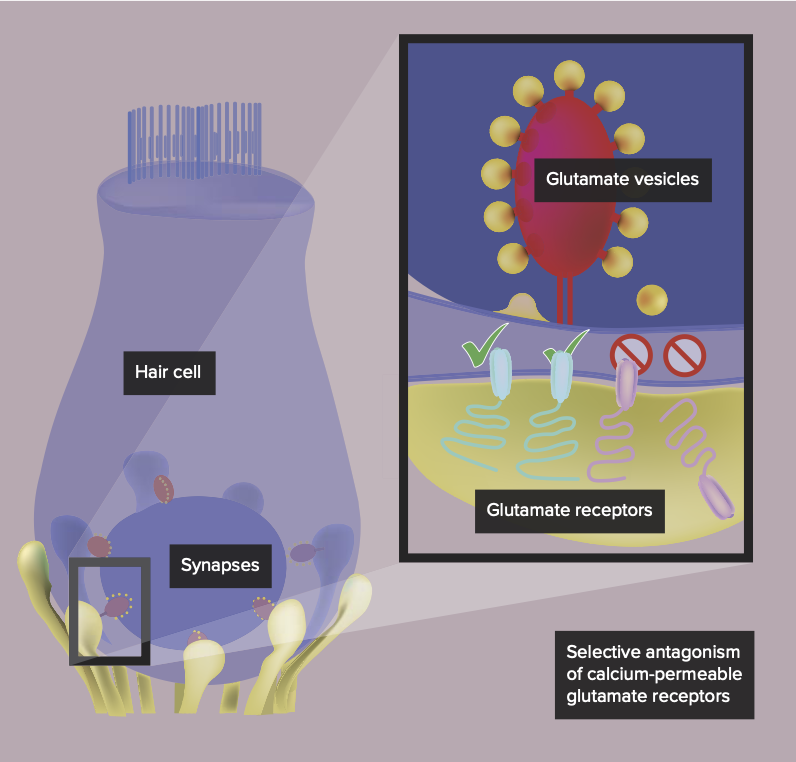
Noise-induced hearing disorders, like hidden hearing loss, in which hair cells survive but synaptic connections to cochlear nerve fibers are lost (a process called synaptopathy), appear to be caused by glutamate excitotoxicity. Glutamate is the chemical messenger responsible for signaling between the sensory hair cells of the cochlea and the nerve fibers that carry sound information to the brain. Without this signal mediated by glutamate, hearing does not happen.
Unfortunately, the deluge of glutamate signaling that occurs in the cochlea during loud sounds can over-excite the nerve fibers, producing toxicity that destroys the synaptic connections permanently.
What if factory workers could take a pill to prevent damage from noise exposures expected during the workday? What if soldiers could take an injection to rapidly intervene after an unexpected noise exposure? Today, hearing loss researchers are developing ways to tamp down glutamate signaling to prevent glutamate excitotoxicity while allowing hearing function to proceed uninhibited.
How can we mitigate noise-induced glutamate excitotoxicity?
Noise-induced glutamate excitotoxicity may be mitigated pharmacologically by inhibiting glutamate signaling in the cochlea. However, such a treatment is made difficult by two main factors.
First, local delivery of drugs to the inner ear is very invasive and not to be done repeatedly, particularly to a healthy cochlea, making systemic delivery the only option. Second, glutamate is the principal chemical messenger for fast synaptic transmission in the entire nervous system. Thus, drugs that target glutamate transmission systemically have intolerable behavioral side effects, which has limited the development of therapies targeting disorders of glutamate signaling, including excitotoxicity.
The role of pharmacological selectivity in cochlear therapy
Recently, researchers have made surprising discoveries making glutamate excitotoxicity in the cochlea a more tractable problem. When glutamate binds to receptors on nerve fibers, the binding opens a channel permeable to positive ions.
During noise exposure, the excess influx of ions into these nerve fibers can produce glutamate excitotoxicity. Researchers discovered that the cochlea uses two main types of these glutamate receptors: some have a large ion channel permeable to calcium, and others have a small ion channel impermeable to calcium.
The trick is to block signaling at the so-called calcium-permeable receptors while allowing signaling to continue at the calcium-impermeable ones, which, in the cochlea, prevents glutamate excitotoxicity while allowing hearing function.
Avoiding temporary hindrance of hearing function while protecting the ear from loud sounds is avoiding an off-target side effect. Although these calcium-permeable glutamate receptors are abundant in the cochlea, they are much less relatively abundant in the brain, which predominantly uses the calcium-impermeable kind under normal conditions. Thus, through pharmacological selectivity on glutamate receptors such as these, it should be possible to avoid side effects coming from the brain while preventing glutamate excitotoxicity in the cochlea.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.