Amit Walia, Matthew Shew, and Craig A Buchman from Washington University School of Medicine, guide us through hearing and auditory research predictive models for cochlear implant outcomes in adults
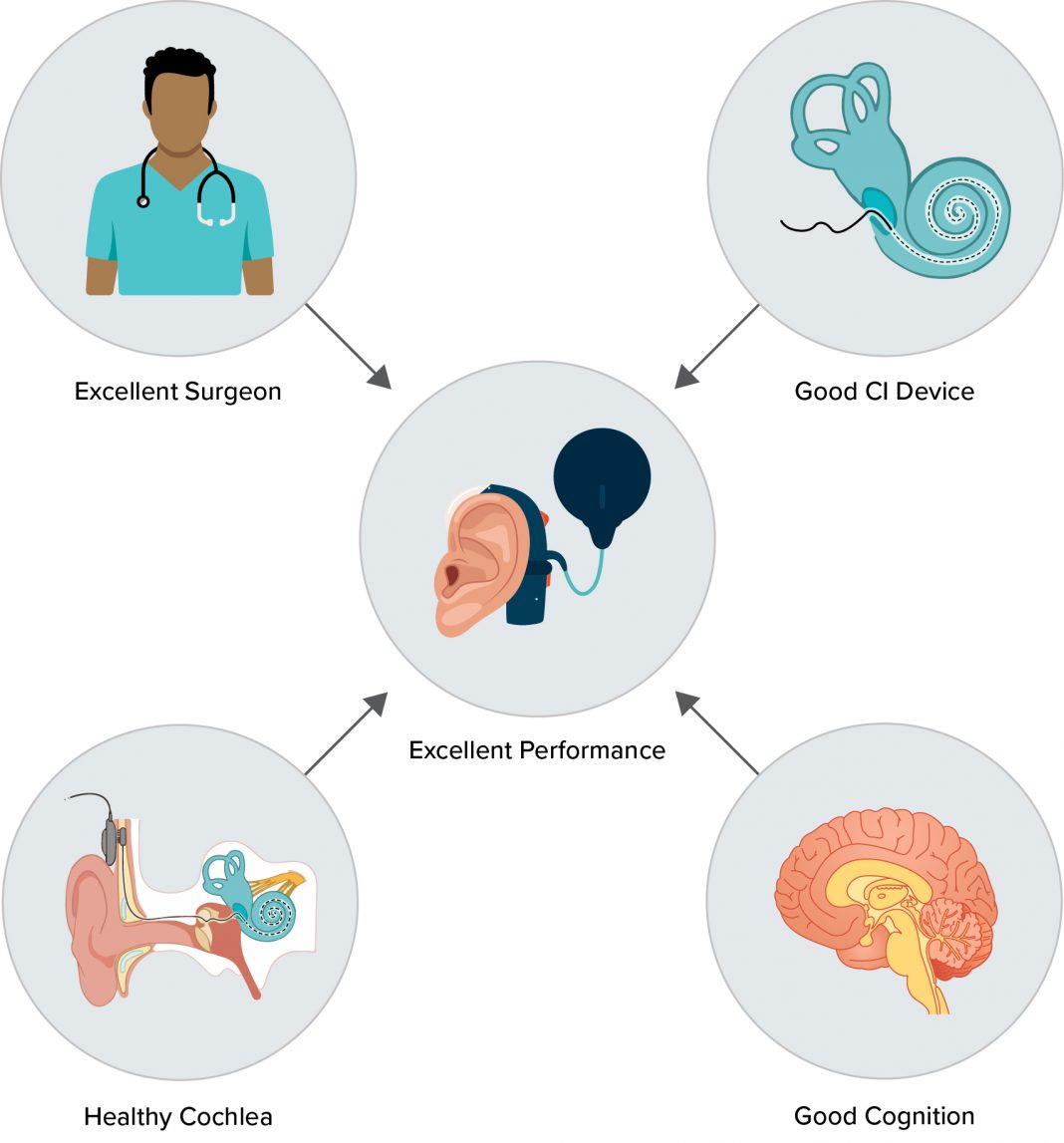
Hearing loss, affecting 1.5 billion people worldwide is the most prevalent sensory disorder. While hearing aids assist those with mild to moderate-severe loss, cochlear implants (CIs) are essential for severe to profound cases to restore hearing. Yet, the wide variability in CI users’ speech comprehension outcomes presents a significant challenge, affecting patient expectations and the identification of candidates for early rehabilitation and device optimization.
Addressing this, our research over the past decade has focused on developing predictive models to understand CI outcomes by examining critical factors, including demographic variables, electrocochleography, cognitive factors, electrocochleography-based electrode programming, and machine learning techniques. Each of these pivotal topics will be explored in greater detail in a dedicated section throughout the year, aiming to understand pathways to more personalized and effective CI interventions.
Role of demographic, audiological, and surgical factors
Historically, studies from the 1990s identified that longer periods of deafness and older age at implantation negatively impacted CI outcomes. However, recent research involving diverse patient groups and expanded implantation criteria indicates that these factors account for less than 20% of the variability in CI performance. Traditional audiological tests used to determine CI candidacy, such as the consonant-nucleus-consonant (CNC) word test and the AzBio sentences test, while useful for assessing hearing loss severity, are limited in predicting CI success.
Moreover, the evolving standardization of surgical techniques and devices has further reduced the predictive value of these variables. Consequently, the weak correlation between demographic, audiological, and surgical variables with CI outcomes underscores the complexity of accurately forecasting CI success. This complexity highlights the imperative need to identify new biomarkers that more effectively predict CI performance beyond the conventional factors currently considered.
Electrocochleography: A diagnostic tool for evaluating cochlear health
In the past decade, our research has leveraged electrocochleography (ECochG) to gauge cochlear health, recording electrophysiologic responses to acoustic stimuli to evaluate the residual function of hair cells and neural pathways in those with hearing loss. A significant breakthrough was the development of the ECochG-total response (ECochG-TR) as a biomarker for cochlear health, obtained by analyzing acoustically evoked responses at the round window during CI surgery. Using pure tone bursts and fast Fourier transformations, this method explained approximately 46% of CI performance variability six months post-implantation, outperforming traditional predictors. (1-2)
Advancing this methodology, we explored a similar but different measure known as the tonotopic ECochG-TR, measured using intracochlear responses post-electrode insertion. This indicated an even stronger correlation with CI outcomes. (3) This work and others have led to our current NIH/NIDCD-funded study, focusing on trans-tympanic promontory recordings as a predictor of performance. The ultimate goal of this work is to translate these recordings outside of the operating room to the clinic for use as a preoperative prediction measure. These findings affirm the critical role of cochlear health assessment through ECochG in predicting CI performance variability.
Cognitive factors in CI outcomes
Our exploration into CI performance variability also focuses on better understanding neurocognitive factors, such as working memory, attention, and executive function. These “top-down” processes are believed to be crucial for interpreting the distorted speech signals delivered by CIs. Utilizing the Montreal Cognitive Assessment (MoCA) as a basic cognitive measure, we have delved into CI effectiveness in noisy environments. This provides a realistic gauge of a user’s auditory function in everyday scenarios. Initial results reveal that good performance in quiet is necessary but not sufficient to guarantee success in noise.
Interestingly, while ECochG-TR and MoCA scores individually offered limited predictive power for noise performance, their combined analysis in a multivariate model accounted for 45% of performance variability in the noisy setting. (4) These preliminary findings emphasize the importance of good cochlear health and strong cognitive abilities for successfully processing speech in noise. Notably, cognitive factors seemed less influential in quieter environments. Our ongoing research aims to refine these cognitive assessments to enhance predictions of CI outcomes across various listening conditions.
Electrode programming using ECochG for optimal CI performance
Intracochlear ECochG using the electrode contacts for recordings along the array provides an opportunity to create a detailed tonotopic map of the cochlea for each CI recipient by measuring tuning curves for individual frequencies. We hypothesize that an ECochG-derived map could be the most effective strategy for post-implantation electrode programming. Our preliminary findings reveal a modest linear correlation between the amount of mismatch between the manufacturer-provided default frequency allocation map and that derived from ECochG measures, with this mismatch explaining ~26% of the variance in CI performance.
When combined with ECochG-TR (i.e. cochlear health), this approach can explain 62% of the variability in CI performance in quiet settings. This highlights the importance of integrating ECochG-TR, cognitive assessments, and precise electrode programming to understand CI performance variability better.
Conventional statistics and machine learning in predictive modeling
Traditionally, predictive modeling in CI outcomes has relied on conventional statistical methods like linear regression and multivariate modeling. While valuable, these methods are time-consuming and require significant expertise, particularly when interpreting nuanced ECochG responses.
In contrast, machine learning offers a ‘big data’ approach, capable of efficiently handling large datasets and identifying complex patterns. Machine learning’s integration into CI predictive modeling represents an exciting frontier, promising more personalized, accurate, and efficient predictive models. (5) This transition from traditional statistics to machine learning could significantly benefit CI recipients, offering tailored interventions and improved outcomes.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.