Prof Richard M Hall, School of Mechanical Engineering, University of Leeds, explores how oncological engineering is paving the way for new and innovative cancer treatments
The burden of cancer is a constant focus for the UK National Health Service and the public it serves. Over 2.1 million people in the UK are living with cancer(1) and this is predicted to rise to more than 3 million by 2030. Treatments that underpin cancer: surgery (44 % of all cancer patients), chemotherapy (28%) and radiotherapy (27%) all rely heavily on the engineering and physical sciences (EPS). This may include, for example, radiation physics and imaging as well as robotics used in surgery.
Engineering and cancer
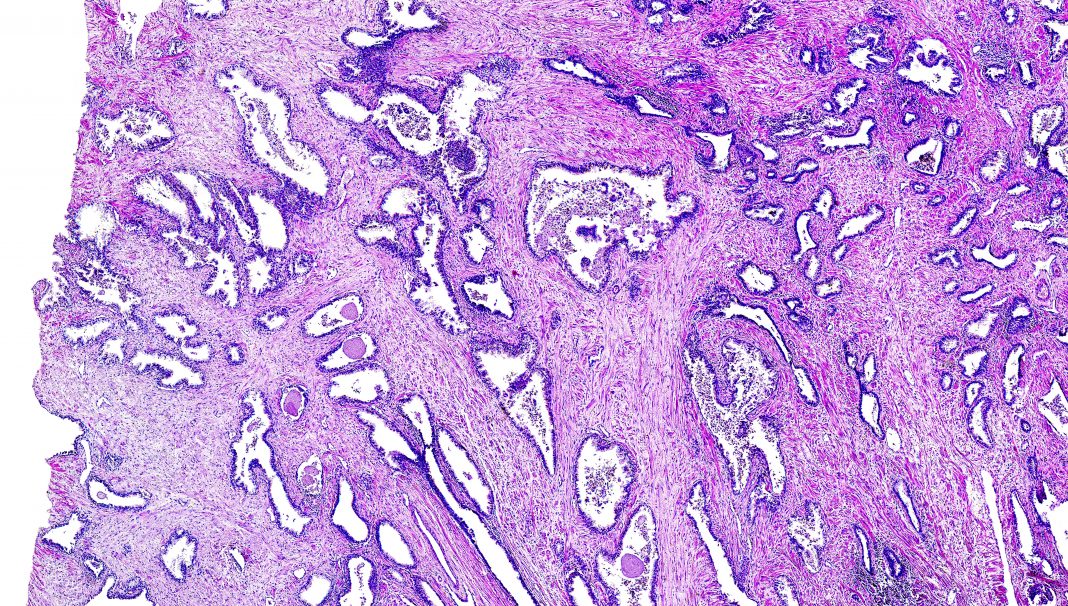
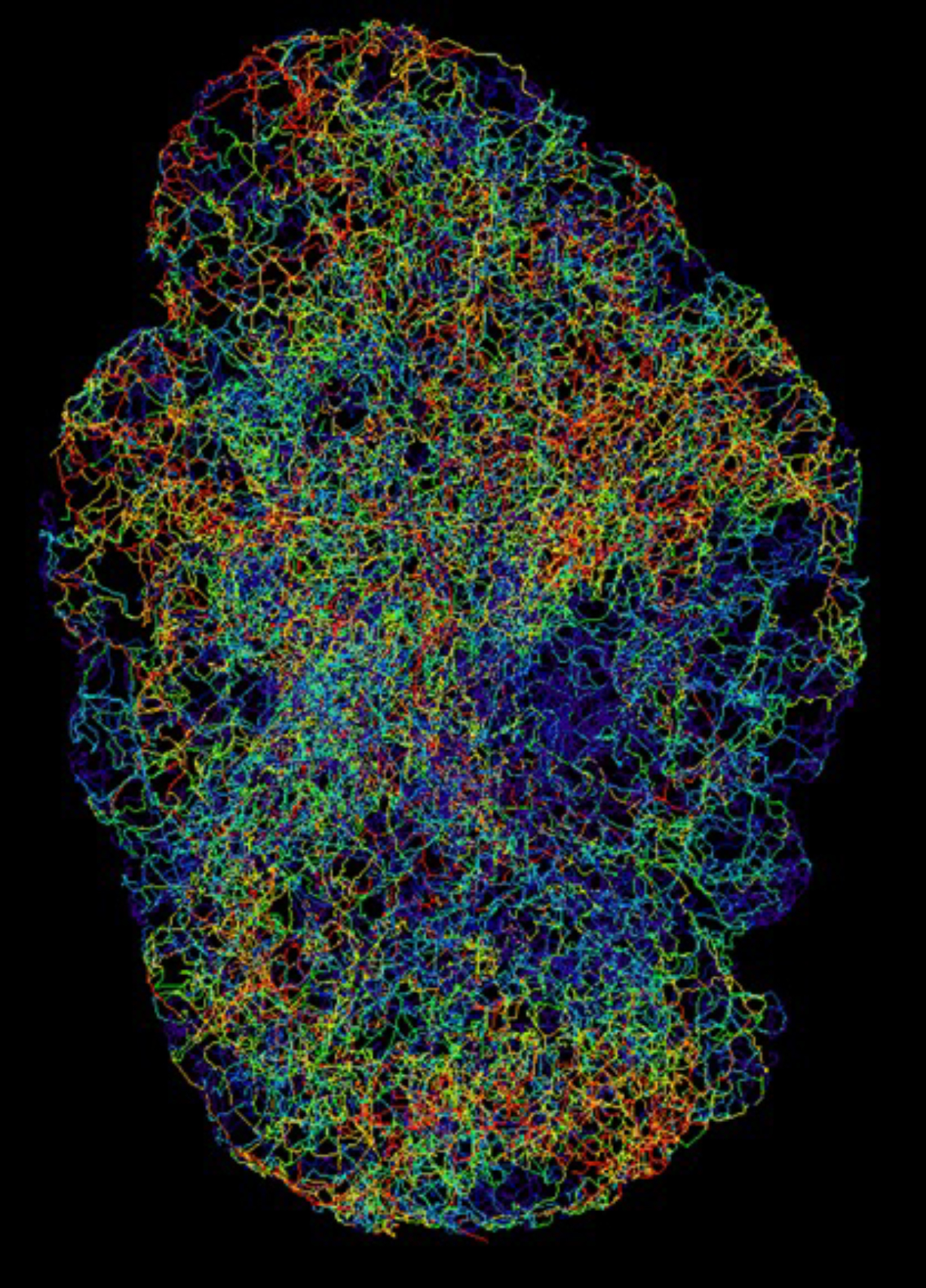
In the discovery domain, important breakthroughs are made by investigating fundamental aspects of the cancer microenvironment, such as fluid flow within tumours that underpins growth and treatment (Figure 1) as well as new ways of treating cancer using novel materials. Also, from a wider perspective, engineering systems enable the following:
- Large-scale drug synthesis, production and deployment
- Software development which enhances the complex management of patients and their interactions with healthcare providers
- Advanced imaging, including the utilisation of machine learning and artificial intelligence
Without these activities, the treatment of cancer patients, now and in the future, would be severely degraded, placing more pressure on health services and increasing the distress of patients and their families.
Innovative cancer treatments require government investment
The skills required to drive forward innovative treatments in cancer call for continued investment from government and industry as exemplified by the ‘Life Sciences Vision’, which recognises EPS as a key player(2). Added to this is the recognition of the need for advanced manufacturing (an engineering enterprise) if new technology’s economic and health benefits are to be maximised across all interventions.
The UK Research Councils currently provide broad provision within cancer, but further development of more holistic, interdisciplinary approaches is required. Added to this are the significant barriers to enabling this potential, especially in terms of professional development where further workforce planning and training would be beneficial. These challenges affect the NHS’s ability to deliver key goals post-pandemic(3), including the drive to reduce cancer waiting lists(4).
This is exacerbated by the fact that the UK has a shortage of engineers and not all are entering engineering jobs, since other avenues which require advanced quantitative skills are seen as more career friendly and often have better renumeration packages. As well as addressing pay and conditions, a first step would be to create CDT-style training and fellowship programmes based around specific cancer challenges within EPS departments in universities but partnered with NHS providers and industry. These would deliver doctoral candidates and early career researchers with the core skills to allow a seamless transfer out of the University sector.
Beyond technological deployment of cancer treatments
EPS may be only one requirement for the successful investigation and ultimate delivery of cancer treatments, as many of the barriers to deployment are not technological. Even here, engineers have a wealth of skills and experience within other domains where interdisciplinary research is key. Engineers work with stakeholders, especially patients, to deliver solutions that meet an agreed set of requirements within a more systems design/engineering approach.
This continued interaction from the point of conception is hugely important, even in the early discovery stages of research, where missed or ill-defined requirements may lead to delays in trials, expensive modifications and reduced market opportunities.
Regarding the research landscape, the creation of UKRI is a positive move that should allow the development of more challenged-based interdisciplinary research. New cross-funder activities help in this respect, and the recent NIHR-EPSRC call for Systems Engineering Innovation hubs for Multiple Long-term Conditions (Seismic) recognises the contribution engineering can make, not just in technology but also in ways of thinking(5).
Oncological engineering case study
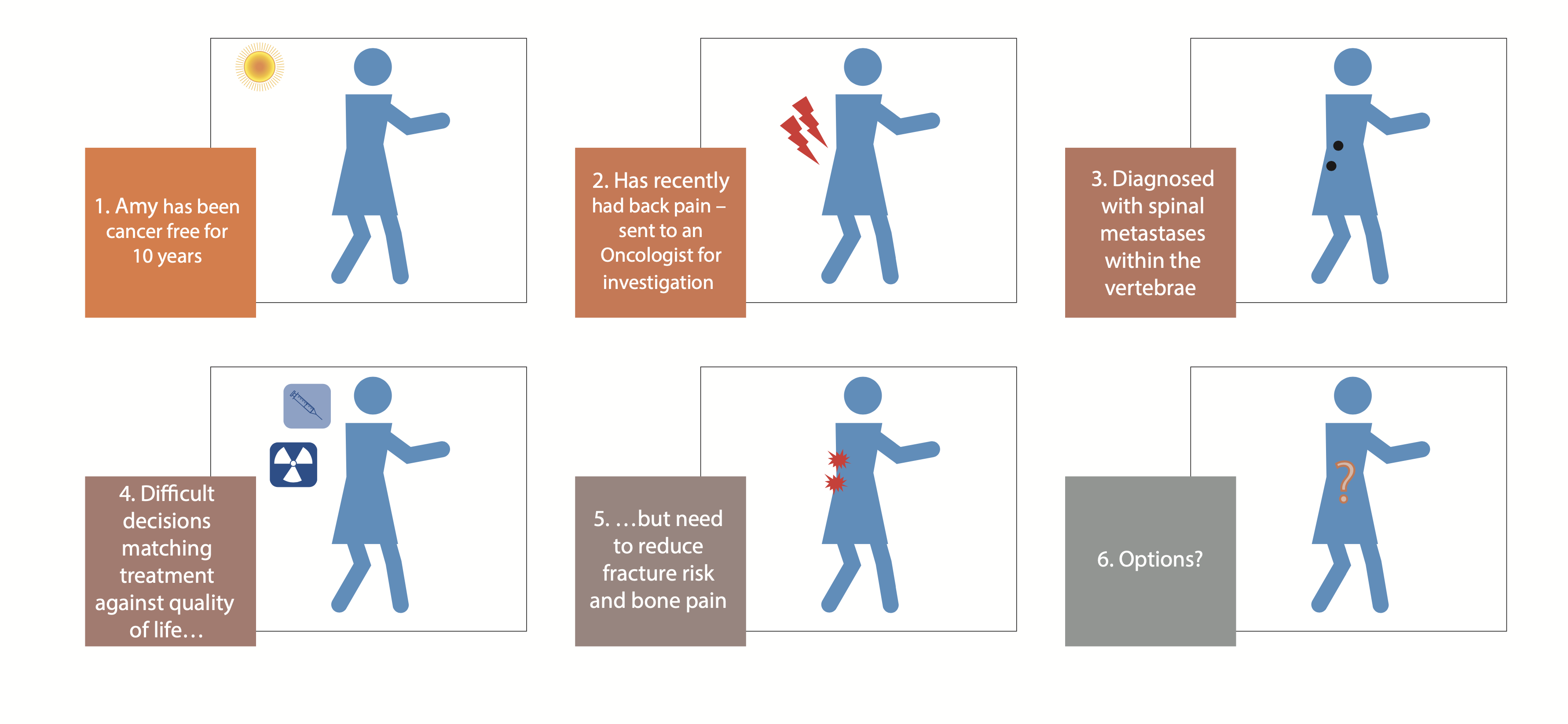
A rising challenge facing the NHS is that of metastatic cancer where the cancer spreads to other organs away from the primary site. These tumours may arise several years after a patient has been declared ‘cancer free’. An increasing concern is that these metastases frequently occur in bone, particularly the spine (vertebrae). These tumours tend to weaken the bone leading to devastating fractures, pain, and the possibility of spinal cord injury, all of which have a severe impact on quality of life at the end of life (Figure 2). Current treatments following fracture of bones in the spine affected by secondary tumours can be complex.
Medical professionals have called for the early detection of secondary tumours in bone and minimally invasive surgical techniques to prevent fracture whilst maintaining the patient’s good quality of life at a time when many older patients want to ‘sit their grandchildren on their knee’.
The UKRI-funded Oncological Engineering research project (OncoEng)(6) aims to model these types of secondary tumours and develop a new type of implant to be inserted minimally invasively. This innovative implant displays novel properties and is designed as a patient/lesion-specific device. In this research, we are collaborating with clinicians, patients, and other stakeholders to ensure optimal approaches to these early stages of development of the intervention.
It is often said that EPS is a forgotten domain in cancer and clinical sciences, a notion reflected in the recent public lecture sponsored by the IPEM entitled ‘Hiding in Plain Sight:
The Unseen Impact of Engineering in Healthcare(7). If we are going to be successful in developing and deploying new diagnostic tools and treatments for cancer, then EPS needs greater recognition as a crucial element of an interdisciplinary approach. Interventions that acknowledge and utilise this wider perspective lead to better innovation and are, first and foremost, in the patient’s best interests.
References available on request


This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.