Integrative oncology gives patients the tools to not only make the environment as inhospitable to cancer as possible – it also empowers patients to take some control back after receiving a cancer diagnosis
“You have cancer” are three words no one wants to hear. Yet, thousands of people every day worldwide are faced with those exact words – and the fear, anxiety, and loss of control that comes with them.
Cancer is a multi-faceted and complex disease, and given the uniqueness of individuals, it is safe to say that no two cancer patients are the same.
Yet healthcare professionals understand at least one universal tenet regardless of the cancer type or the individual – the patient’s body is the environment in which the cancer is attempting to proliferate. Building from that, the body and mind are inextricably linked such that stress perceived by the mind causes physiological changes in the body and affects many aspects of our health. Taken together, this means that how patients treat their bodies and how they manage their mindset affects the environment in which the cancer wants to grow. Integrative oncology gives patients the tools to not only make that environment as inhospitable to cancer as possible – it also empowers patients to take some control back after receiving a cancer diagnosis.
What is Integrative Oncology?
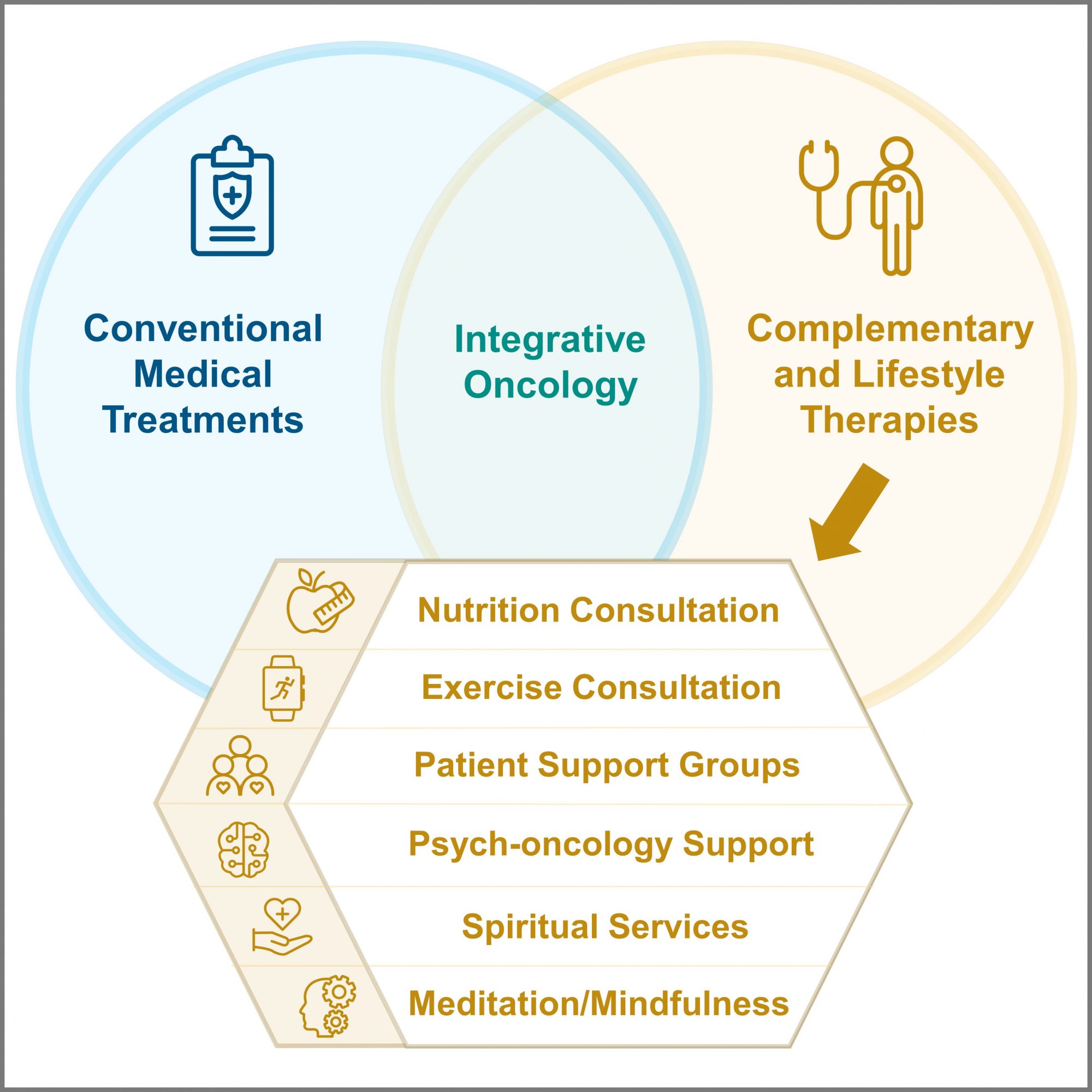
As defined by C.M. Witt et al in the Journal of the National Cancer Institute, integrative oncology is “a patient-centred, evidence-informed field of cancer care that utilizes mind-body practices, natural products, and/or lifestyle modifications from different traditions alongside conventional cancer treatments.” Patients can use numerous complementary and lifestyle therapies, which I will refer to as complementary therapies for simplicity. Some of the most common are nutrition and exercise counselling, psycho-oncology support (therapy), meditation/mindfulness, spirituality, patient support groups, yoga, massage, acupuncture, reiki, music or art therapy, and tai chi or qi gong. There are many other complementary modalities, but these twelve are a good representation of the needs of mind, body, and soul.
What are the benefits of Integrative Oncology?
Beyond giving patients back some control after diagnosis, there are numerous clinical benefits. Many studies have been published about improved patient-reported outcomes compared to using medical treatments alone. In a recent survey from the Samueli Foundation of over 1,000 US cancer patients, over 50% strongly agreed that integrative oncology improves overall well-being during and after treatment.(1) Among breast cancer patients, a 2021 survey showed this belief in improved well-being is even stronger at 63%.(2)
In addition, there is also wide-spread acceptance that using complementary therapies helps patients manage the often-toxic side effects of treatment. In the Samueli study, 51% of patients and 66% of treating oncologists strongly agreed with this sentiment.(1) Decreasing adverse events in turn allows patients to adhere to medical treatments, decreases emergency room visits, and decreases hospital admissions due to treatment complications.
Finally, and most importantly, combining complementary therapies with medical treatments has proven to improve breast cancer patients’ survival odds. There are numerous studies that focus on exercise improving both progression-free and long-term survival, including in breast cancer.(3) In addition, the 2021 research I led showed that hospitals in the US meeting a minimal threshold of integrative oncology involvement have increased 5-year overall survival odds for their breast cancer patients compared to hospitals below the threshold.(4)
So, why has this life-improving approach not been widely adopted?
Healthcare professionals and patients each have their set of barriers, but they are all able to be overcome with concerted efforts. Education of both parties is key.
In the same recent Samueli study, US Oncologists and patients were asked about barriers to increased adoption of complementary therapies. Oncologists cited lack of insurance reimbursement (49%), lack of staff (39%), a misperception that patients are not interested (32%), and a lack of time to fit these options into patient conversations (31%).(1) The US intuitions that have been successful have one or more champions who are educated and passionate about integrative oncology, partner with foundations like Samueli as a vetted source for patient education, set up processes for triage and referral of patients to specific modalities, and raise funds through philanthropic efforts. They also find innovative ways to manage the US payer system; for example, using group visits to achieve partial reimbursement. If policymakers were exposed to the data and educated on the clinical outcome benefits, perhaps coverage of these life-improving modalities would increase.
Cancer patients reported a lack of knowledge about complementary therapies (26%) and their hospital not offering them (26%) as the single largest barriers to complementary use. Being focused on medical treatment and not having the money to pay for complementary therapies were also cited by more than 20% of cancer patients.(1) The patients that are successful are provided gentle facilitation from their treating institution or from a patient advocacy group – which includes education on the benefits of adding complementary therapies to the medical treatment, access to professionals that can consult and/or deliver the services, and funding to help with payment during active treatment.
What Are the Recommendations to Policymakers and Institutions?
There is clear and objective value in investigating the evidence base for integrative oncology. Look to organizations like the Society for Integrative Oncology (SIO) and the American Society of Clinical Oncology (ASCO) who are jointly publishing guidelines that show how to apply whole-person care to cancer patients.(5) Conduct the analyses needed to justify the investment of funding integrative care for patients – increased treatment adherence contributes to improved outcomes, decreased cancer patient ER visits and hospital admissions lowers healthcare system costs, and increased survival odds is the endpoint everyone is seeking.
Finally, provide a seat at the table to advocates like me who speak on behalf of many cancer patients. There is more that can be done institutionally to support people with cancer as more than just patients taking medical treatments. We are individuals who have needs across the constructs of mind, body, and soul – and we want to do everything we can to help our fellow patients live long into survivorship.
References
- https://drwaynejonas.com/2022cancersurvey
- Crudup, T et al. Breast Cancer Patients Desire More Whole Person Integrative Oncology Support. https://www.iqvia.com/locations/united-states/library/white-papers/breast-cancer-patients-desire-integrative-oncology-support. Oct 2021.
- Cannioto RA, Hutson A, Dighe S, et al. Physical Activity Before, During, and After Chemotherapy for High-Risk Breast Cancer: Relationships With Survival. J Natl Cancer Inst. 2021 Jan 4;113(1):54–63.
- Crudup T, Li L, Dorr JW, et al. Breast Cancer Survivorship and Level of Institutional Involvement Utilizing Integrative Oncology. J Oncol. 2021 Dec 18;2021:4746712. doi: 10.1155/2021/4746712.
- Lyman GH, Greenlee H, Bohlke K, et al. Integrative Therapies During and After Breast Cancer Treatment: ASCO Endorsement of the SIO Clinical Practice Guideline. J Clin Oncol. 2018 Sep 1;36(25):2647-2655. doi: 10.1200/JCO.2018.79.2721.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.