Professor Hamdy Awad, MD, FASA, from the Ohio State University Wexner Medical Center, examines the dangers of aortic aneurysm surgery and the importance of continued research towards eliminating paralysis
Aortic aneurysmal disease is a rapidly growing problem in the United States. Ruptured aortic aneurysm is the 12th leading cause of death in the U.S. with 43,000–47,000 deaths per year (1).
Risk factors associated with aneurysmal disease include old age, smoking, male sex, and a family history of aortic aneurysm. Aortic aneurysms inevitably rupture due to their thin and weakened walls, resulting in massive internal bleeding, which is usually fatal. This necessitates timely surgical intervention.
Aortic disease and the dangers of aortic aneurysm surgery
Currently, the only treatment for aortic disease is surgical repair. During the surgery, blood flow in the aorta is temporarily interrupted. Since the aorta gives rise to blood vessels that supply the spinal cord, one of the most feared complications of aortic surgical repair is postoperative leg weakness and even paralysis.
Paralysis costs $2.3 million per patient in their lifetime and there is an ongoing need to tackle this problem both in and out of the clinic (2). Patients who experience any spinal cord injury after surgical repair have a significantly lower 1-year survival compared to patients who do not experience spinal cord injury (3).
Paralysis following aortic surgical intervention has been recorded since the procedure’s advent. Before the first aortic repair, Dr. Alexis Carrel, a Nobel prize-winning surgeon who pioneered many vascular techniques, predicted that “the main danger of the aortic operation does not come from the heart or from the aorta itself, but from the central nervous system.”
The danger of paraplegia following surgical repair
Dr. Carrel’s prediction was proven correct when the first recorded instance of paraplegia following surgical repair occurred in 1951, which was also the first successful resection of an aortic aneurysm.
Dr. John L. Doppman, former director of NIH Clinical Center for Imaging Sciences, stated in 1993 that paraplegia after aortic aneurysm surgery is a “Russian roulette” for vascular surgeons. He also stated that “as long as we don’t understand the pathophysiology, we can propose no reasonable remedy.” This point remains salient due to the current lack of scientific knowledge on the mechanism of neurological damage causing paralysis.
The past fifty years of research have not yet resulted in a pharmacological treatment to prevent paralysis, and there exists no approved mechanistic therapeutic intervention to prevent this dreaded complication. To advance scientific knowledge, our group developed and published animal models to model surgical aortic intervention. Furthermore, investigation of the mechanism of neurological damage to the spinal cord shall follow to develop and test therapeutics for potential clinical use.
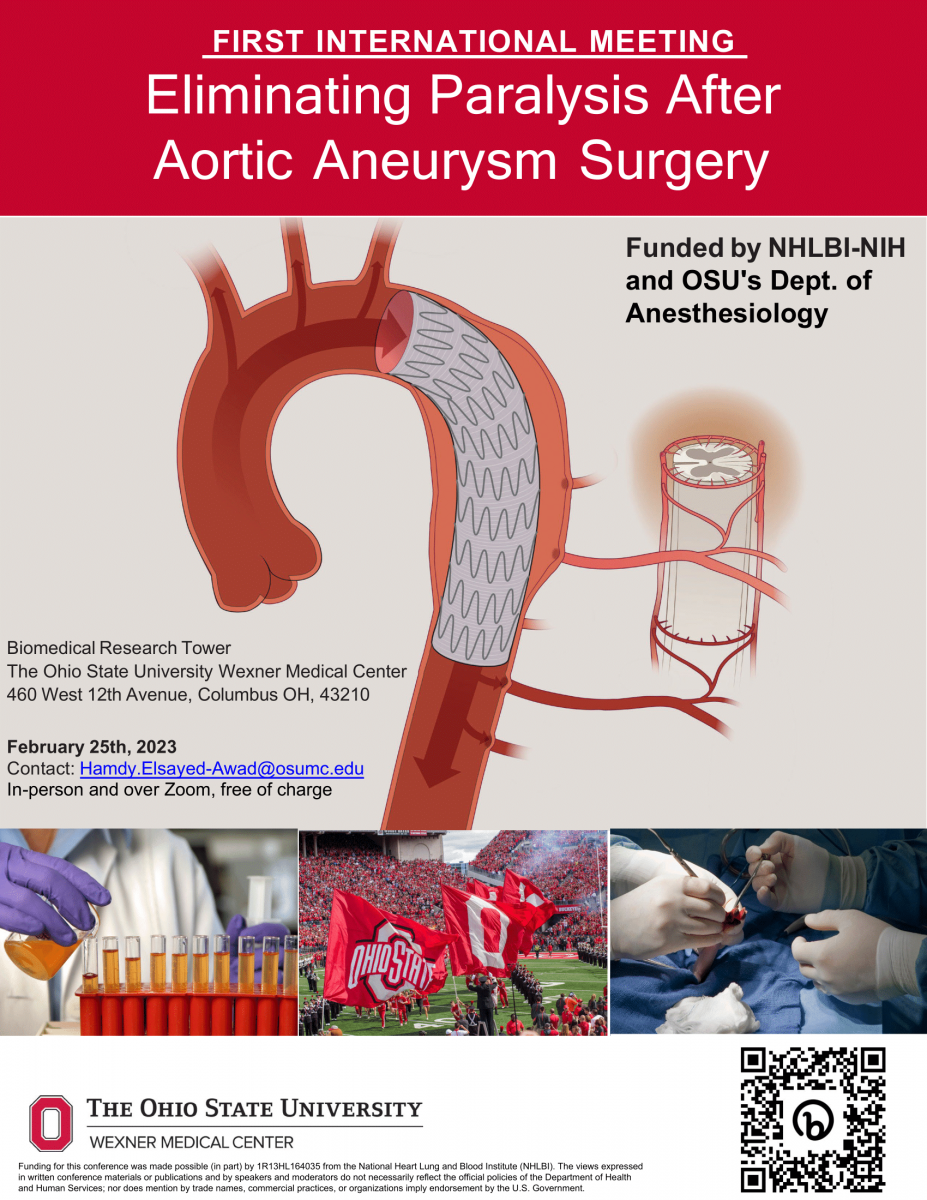
International meetings towards “Eliminating Paralysis After Aortic Aneurysm Surgery”
Recognizing the need for worldwide collaboration, in February 2023, we hosted the first multisession, international meeting at The Ohio State University Wexner Medical Center, titled: “Eliminating Paralysis After Aortic Aneurysm Surgery”. This meeting was funded in part by the National Heart and Lung Institute in the U.S.
The meeting was attended by 400 individuals from over 25 countries, including Dr. Joseph Coselli, an eminent aortic surgeon who presented “The Past, Present, and Future of Ischemic Spinal Cord Injury and Paralysis after Aortic Aneurysm Surgery.” Two patients were invited to discuss personal experiences with paralysis after aortic aneurysm surgery, which served as a poignant and humbling reminder to the physicians and scientists addressing this issue.
The future of paralysis research
The meeting revealed multiple future directions of research in spinal cord ischemia. In the Basic Science Solutions to Eliminate Paralysis session, Dr. Arthur Burghes, a researcher of the molecular basis of neuromuscular disorders, discussed efforts to develop a small molecule to achieve the neuroprotective effects of hypothermia without its maladaptive responses.
Dr. Esmerina Tili highlighted the role of microRNAs as biomarkers for ischemic spinal cord injury. Dr. Jim Vaught, former editor-in-chief of Biopreservation and Biobanking, discussed the standard of care of collecting biofluids from patients with and without paralysis. Upon collection, analysis can be performed to compare biofluids between experimental groups.
The omics approach for collected biofluids may help further the understanding of pathophysiology.
Two objectives emerged from the final session’s discussion about the effectiveness of the prophylactic spinal drain in patients after thoracic endovascular aortic repair who are high-risk for spinal cord injury.
One is that there needs to be a global effort to understand and eliminate this dreadful surgical complication due to its multidisciplinary nature. Two, the omics analysis of biological fluids is key to developing biomarkers and future therapeutic treatments.
NO disease more conducive to clinical humility than aneurysm of the aorta
William Osler’s statement still holds true today, “There is NO disease more conducive to clinical humility than aneurysm of the aorta.”
We hope to continue studying small- and large-animal models of pathophysiology and to employ genomics and systems biology to characterize the mechanisms of spinal cord injury and paralysis after aortic aneurysm repair.
References:
- Beckman JA. Aortic aneurysms: pathophysiology, epidemiology and prognosis. In: Creager MA, Dzau VJ, Loscalzo J, editors. Vascular medicine. Philadelphia, PA: Saunders Elsevier; 2006.
- (2019). How Much Does Paralysis Cost? The Beasley Firm LLC.
- Awad H, Alcodray G, Kelani H, Essandoh M. Is It Too Much to Request a Formal Neurology Consultation After Thoracic Endovascular Aortic Aneurysm Repair?
J Cardiothorac Vasc Anesth. 2021 Apr;35(4):1253-1254. doi: 10.1053/j.jvca.2020.09.084. Epub 2020 Sep 6. PMID: 33023814; PMCID: PMC8715520.
Acknowledgements:
Chris Janyelle Auman1, Katherine Choi, BA2, Andrew Denney, BS2, Bradley Gigax1, Alim Habib, BS2, Rafia Baig1, Amar Dabbagh1, Brendan Sieber, BS2, Jacob Christofi, MSc2, Alexander Efanov, BS2, Hamdy Awad, MD, FASA3
- The Ohio State University, Columbus, Ohio
- The Ohio State University College of Medicine, Columbus, Ohio
- Department of Anesthesiology, The Ohio State University Wexner Medical Center, Columbus, Ohio

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.