Prof. Giovanni Brandi and Dr. Simona Tavolari investigate the prevalence of asbestos fibres in drinking water around the world
For decades the health risks of asbestos have been discussed among academics, companies and countries, but nowadays its harmfulness is recognised worldwide. Still in 1997, when asbestos use was banned in French, Canada (the main producer of chrysotile) sustained its innocuity; 3 years later, the carcinogenicity of chrysotile was set off by the World Trade Organization.
While sophisticated estimates have evaluated the link between the number of inhaled fibres and the risk of asbestos-related diseases, a hidden source of asbestos exposure remains almost ignored: the water. This potential source represents a challenge in Western societies, as it poses strong social and political questions. Indeed, unlike airborne asbestos dust, that one cannot avoid inhaling and whose source is often unknown, the source of fibres in water is frequently known, and drinking polluted or safe water is a matter of choice. After some studies in the USA fifty years ago evaluating the presence of asbestos fibres in drinking water, a scientific silence has fallen on the possible health risks of asbestos in the water. On the Western Coast of the USA, the primary (and no modifiable) source of polluted water is asbestos rocks. A different scenario occurs in Europe, where the main source of polluted water is pipes built in asbestos-cement; in Italy, over 125,000 km of asbestos-cement water pipes have been estimated and in the UK over 257,000 km. The only conclusion coming from the American agency US-EPA has been the introduction of 7 million fibres (>10μm) as the threshold value associated with an increased risk of developing intestinal polyps; however, this threshold value has been defined only in rodent models.
What lesson can we borrow from the mesothelioma experience?
An accurate analysis from the Italian National Mesothelioma Register revealed that only 80% of mesotheliomas show a previous asbestos- exposure; in the remaining cases, the source of exposure is unknown, suggesting hidden environmental sources. The risk of mesothelioma follows a stochastic model. Some authors suggested that a threshold value of “fibre saturation” of the pleural spaces exists (beyond which the risk shouldn’t increase), whereas the Italian Consensus Conference on Mesothelioma certified a strong correlation between exposure and risk level (doubling the incidence, or shortening the time of disease development, at higher levels compared to lower levels of exposure).
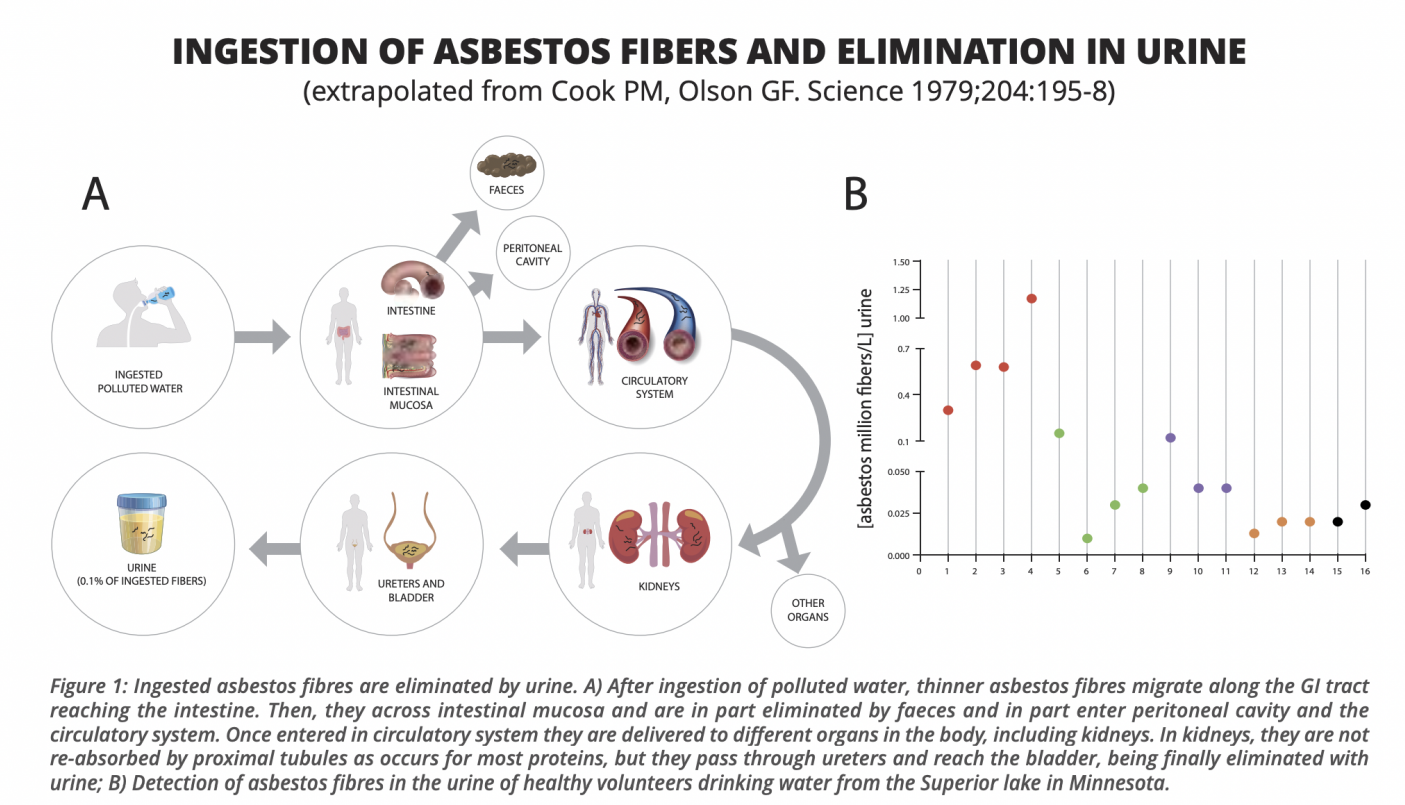
Figure 1: Ingested asbestos fibres are eliminated by urine. A) After ingestion of polluted water, thinner asbestos fibres migrate along the GI tract reaching the intestine. Then, they across intestinal mucosa and are in part eliminated by faeces and in part enter peritoneal cavity and the circulatory system. Once entered in circulatory system they are delivered to different organs in the body, including kidneys. In kidneys, they are not re-absorbed by proximal tubules as occurs for most proteins, but they pass through ureters and reach the bladder, being finally eliminated with urine; B) Detection of asbestos fibres in the urine of healthy volunteers drinking water from the Superior lake in Minnesota.
Despite these conclusions are considered valid for mesothelioma only (where asbestos represents the almost unique risk factor), it is conceivable that they can be applied also for other asbestos-related cancers (although this hypothesis is more difficult to demonstrate, due to the number of confounding risk factors in these diseases). As asbestos carcinogenesis is driven by both genotoxic (direct DNA damage) and non-genotoxic (oxidative stress increase, epigenetic and others) mechanisms, its role is poorly explainable by toxicology, which postulates a threshold effect below which there is no estimable risk.
If for pleural mesothelioma there is agreement that fibre uptake occurs almost exclusively by inhalation (with the preliminary mandatory passage across the pulmonary alveoli), for gastrointestinal (GI) cancers it can occur by inhalation (for clearance of airborne asbestos and subsequent swallowing) and ingestion (water and diet). The relative risk (RR) of developing asbestos-related cancer is variable among various cancer types: 5-50 times for mesothelioma (case-control studies); 2-5 times for lung (case-control studies); 1.16 times for stomach and colon (meta-analysis) (IARC monograph 100, 2012). A more accurate re-analysis, correlating colon cancer risk to the level of asbestos exposure, showed an increased risk of up to 1.38 times for high levels of exposure. This trend is similar to that observed for mesothelioma: more exposure, more risk in less time. Furthermore, an Australian cohort study on about 1 million people living in asbestos-exposed homes showed a colorectal cancer RR of 1.7 in women. Since, intuitively, asbestos fibres reaching the GI tract can cause damage primarily to these organs, the first obvious question is: is there any evidence that ingested fibres may be absorbed by the GI mucosa? An important, but often ignored, a study published in Science in 1979, definitively clarified this point. In healthy volunteers drinking water from the Superior lake in Minnesota (widely contaminated with asbestos), fibres were detected in urine, and their presence was observed for at least 2 months after the last intake.
The concentration of asbestos fibres in urine was about 0,1% of those ingested, suggesting that they can be absorbed by the GI mucosa and in particular the colon (Figure 1). In another study, up to 36 million/100gr of asbestos fibres were found in fish reared in an artificial pond near Milan (Italy), built with cement-asbestos material. These animal studies have undoubtedly shown that fibres can penetrate the intestinal mucosa and migrate to peritoneal sierosa, causing peritoneal mesothelioma. This is of particular interest as a meta-analysis of 20 years ago reported that a variable proportion of mesotheliomas had a peritoneal origin and that while for pleural mesothelioma asbestos exposure induces a linear risk increase, for peritoneal mesothelioma the increase is quadratic.
How do ingested asbestos fibres represent a significant clinical risk?
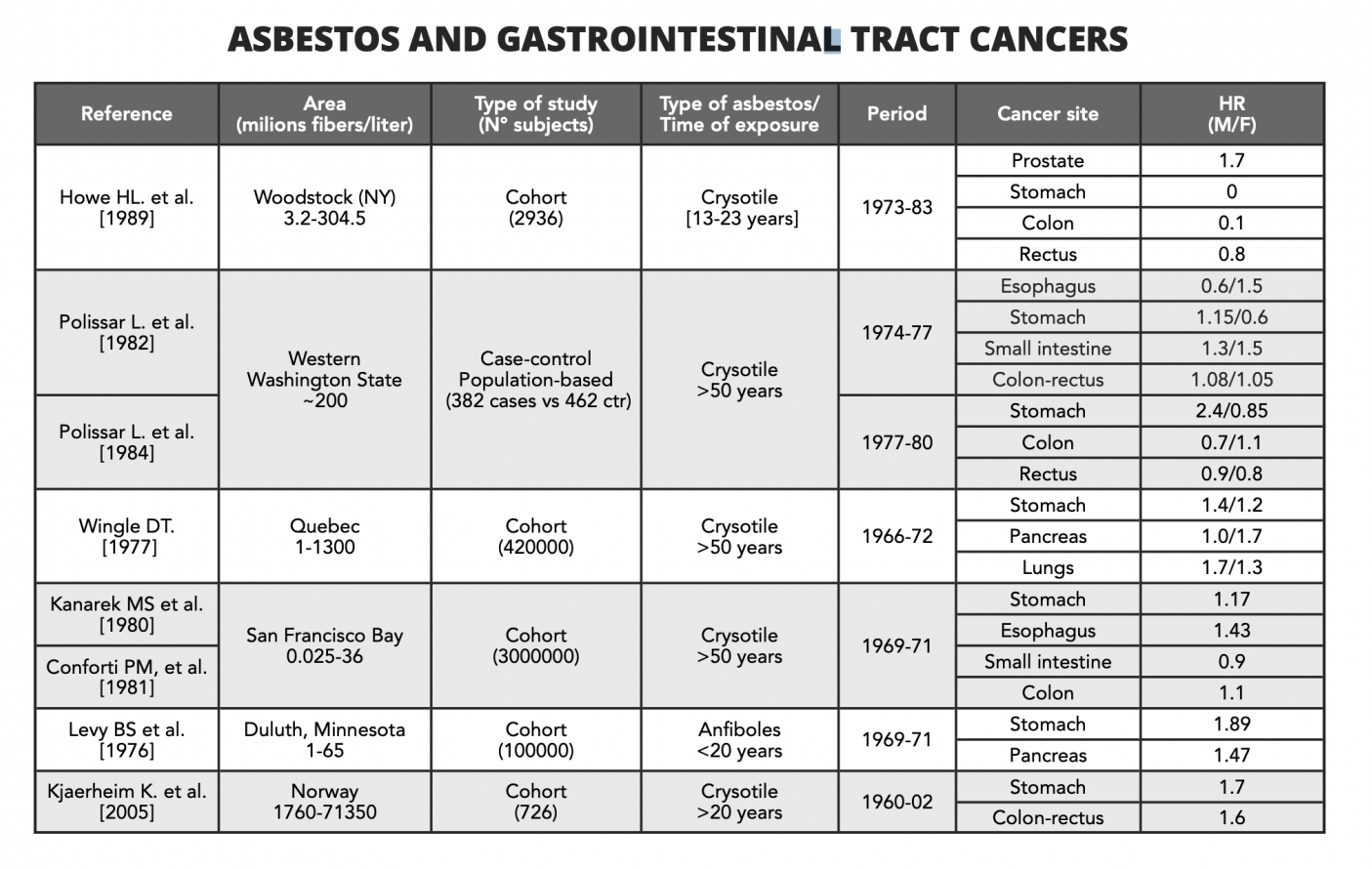
In the 1980s, some ecological studies in North America correlated the incidence/mortality from GI cancer with asbestos exposure in residing populations (Table 1). However, these studies have intrinsic biases due to the misclassification of exposure that: a) is not usually assessed by geographical studies using the residence as a surrogate for exposure; b) is of short duration compared to the long latency time for cancer development; c) requires extremely large samples to detect rare diseases (as cancer) linked to low level of exposure; d) confounding factors (as occur in GI cancer genesis) are not considered. Some of these studies resulted in negative association, but the largest cohort study in San Francisco Bay showed a significant increase in stomach, oesophageal and colon cancers, that was directly correlated to the number of ingested fibres with water. In another Canadian cohort study, subjects exposed to large amounts of fibres (1.2 x 109/L) also showed an increased mortality rate from the stomach and pancreatic cancer compared to the cohort with fewer fibres in water. A further small cohort study, with very high levels of exposure (> 1.8 x 109/L) and a long follow-up, showed an increased incidence of gastric and pancreatic cancer in lighthouse keepers.
Case-control studies are usually more appropriate than cohort studies to capture associations between low exposures and rare events; however, the only study on this issue resulted in negative. This can be due at least to two biases: the small number of cases and controls (<400) and the census section deficit which resulted in the same asbestos exposure between cases and controls. In 2006, a review of 42 cohort studies conducted by IOM of the National Academy of Science certified that the level of evidence was inadequate to infer either the presence or the absence of a causal relationship between asbestos and GI tract cancers. More recently, a close correlation has been demonstrated between the intake of filtered beer (with filters containing asbestos) and oesophageal adenocarcinoma, a tumour with the same epidemiological trend and similar molecular characteristics as mesothelioma.
In the Netherlands, up to 33 million fibres/L have been detected in drinking-water supplies and the Yunnan region (China) up to 42 million fibres/L. In Italy, a progressive increase of fibres has been registered in the last 20 years in drinking water, with peaks over 100,000 fibres /L in Modena city. All these observations strongly suggest that the issue of asbestos in the water remains open and that it has been closed too quickly, not applying (imprudently) a precautionary principle. The resolution of the European Parliament of 14th March 2013, which urges the EU to monitor asbestos in drinking water and the potential health risks, has however shown that politics (at least for once) has proven more sensitive than academics in protecting public health.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


