Shaw-Ruey Lyu, Professor from Dalin Tzu-Chi Hospital, Tzu-Chi University, says that the knee health promotion option and cell therapy are a perfect combination for knee osteoarthritis
Knee osteoarthritis background
Knee osteoarthritis (knee OA) is commonly but mistakenly referred to as a degenerative process of the knee. The mainstream medical community has devoted uncounted resources and talents to identifying the cause of knee OA, but that effort has only produced controversial results.
Consequently, sufferers of knee OA have not been able to rest, and the deteriorating course of knee OA symptoms, which typically start from stage I and worsen to stages II, III, IV, and V, puts the patients through increasingly agonising pain and discomfort.
The mainstream medical community collectively has tried to offer relief to their knee OA patients, such as nonpharmacological interventions, systemic drug treatment, intra-articular therapies ranging from corticosteroids to hyaluronans to more recently platelet-rich plasma, and more invasive surgical procedures such as arthroscopy or corrective osteotomy.
These treatments are the best they offer after spending billions of dollars on R&D over the decades, but these treatments have been repeatedly shown to be sorely inadequate. Many patients eventually require knee replacements, which are permanent but far from ideal.
Improved treatment: KHPO
Once a mainstream orthopaedic surgeon, I am now an advocate for improved treatment of knee OA based on my discovery of a neglected cause of knee OA, the Medial Abrasion Phenomenon (MAP). (1)
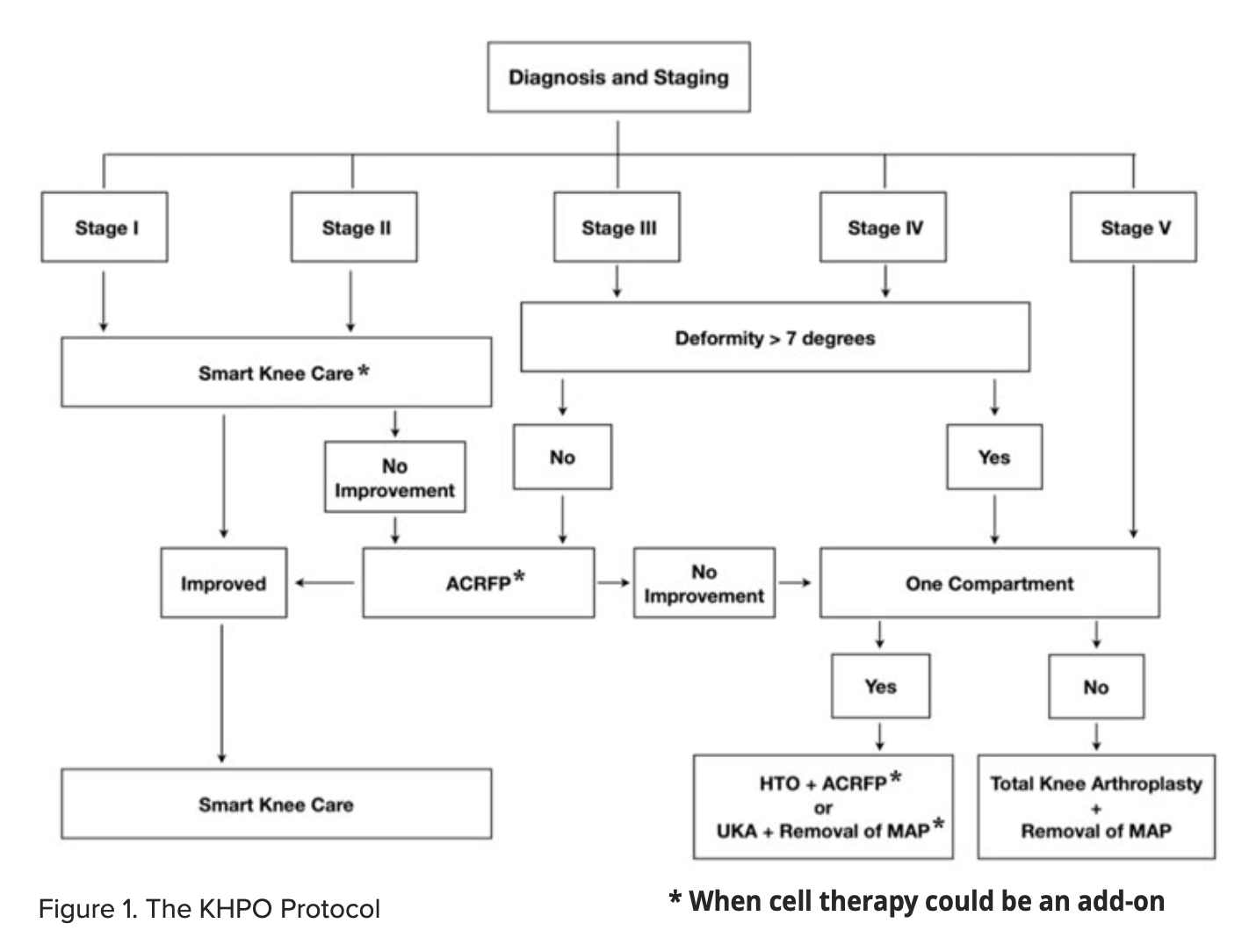
My treatment differs from the mainstream treatment in two significant aspects: the Lyu treatment 1.) aims at diminishing the MAP while the mainstream treatment does not, and 2.) is less invasive. Over 15,000 patients have benefited from our treatment protocol, the Knee Health Promotion Option or KHPO (Figure 1). (2)
Following the KHPO protocol and a special surgical technique, Arthroscopic Cartilage Regeneration Facilitating Procedure (ACRFP) (3), patients no longer need pain medications or other mainstream treatments for relief.
Their knee OA no longer deteriorates. They live their everyday lives again, and most will not need knee replacement. Many patients have seen their damaged knee cartilage regenerated (think thickened). We have seen case after case of cartilage regeneration in our knee OA patients whom we treated under the KHPO protocol – without the assistance of cell therapy (3-5).
Cell therapy and knee health promotion
Adipose-derived stem cells (ADSCs) are stem cells that are found in fat tissues. They are a good source of adult mesenchymal stem cells that can be obtained through surgery (such as arthroscopy) and then separated, cultured, and proliferated using special techniques.
Stem cells are highly modulable and self-renewing and can repair damaged tissues or organs. They are also an autologous, readily available source and pose low rejection risks.
Stem cells possess four major characteristics: they can regenerate and repair, have immunomodulatory effects, differentiate into multiple cell types, and have low immunogenicity. ADSCs treat osteoarthritis in the following ways.
Stem cells inside the joint can be recruited and aggregated. They secrete various anti-inflammatory cytokines to reduce inflammation and pain. They also slow down and prevent cartilage destruction while promoting cartilage regeneration. After injecting ADSCs into the joint, significant cartilage regeneration can be observed in six months.
KHPO/Cell therapy combination
KHPO alone has brought about cartilage repair and regeneration in about 80% of patients after ACRFP (3-5), but we strive for even better results. We added cell therapy to the KHPO treatment protocol to further boost knee cartilage regeneration.
Generally, we will diagnose and assess whether the patient is a good candidate for cell therapy. If so, adipose stem cell samples are acquired, isolated, cultivated, and stored.
The final step is the injection of the ADSCs into the knee joint. Cell therapy could be an add-on for stages I-II patients when doing smart knee care. For patients receiving ACRFP, adipose tissue could be obtained during ACRFP. The timeline of this stem cell therapy process dovetails very nicely with the timeline of recovery of a typical KHPO- treated patient, making the KHPO/cell therapy a perfect combination for treating knee OA.
Acknowledgment: Publication of the present article was supported by the BIONET Corp.
References
- Lyu SR, Chiang CY, Cherng JY, Huang YC, Li CH, Lin YJ, Chang CM, Chau LK. Role of medial abrasion phenomenon in the pathogenesis of knee osteoarthritis. Med Hypotheses. 2015 Aug;85(2):207-11.
doi: 10.1016/j.mehy.2015.04.028. Epub 2015 May 1. PMID: 25957655. - S.R. Lyu, Knee health promotion option for knee osteoarthritis: a preliminary report of a concept of multidisciplinary management, Healthy Ageing Research, 4-34, 2015.
- Shaw-Ruey Lyu, Chia-Chen Hsu and Chih-Wen Lin, Arthroscopic cartilage regeneration facilitating procedure for osteoarthritic knee. BMC Musculoskeletal Disorders 2012, 13:226, http://www.biomedcentral.com/1471-2474/13/226
- Lyu SR, Hsu CC, Hung JP, Chou LC, Chen YR, Lin CW. Arthroscopic cartilage regeneration facilitating procedure: A decompressing arthroplasty for knee osteoarthritis. Medicine (Baltimore). 2022 Sep 30;101(39): e30895.
- Lyu S-R, Hsu C-C, Hung J-P, Chou L-C. Arthroscopic cartilage regeneration facilitating procedure can modify the clinical course of knee osteoarthritis. Journal of Orthopaedic Surgery. 2023;31(2). doi:10.1177/10225536231180331.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


