Professor Richard J. Santen, MD from the University of Virginia, explains the need for retired endocrinologists returning to work to manage patients with diabetes in America’s rural underserved areas, including a comment on telemedicine
Rural, financially challenged areas in the United States lack endocrinologists to help manage patients with diabetes mellitus. One solution is to encourage retired endocrinologists to return to practice part-time and use telemedicine to evaluate and treat these patients. In addition, retired endocrinologists have acquired much wisdom about diabetes management over their years of practice.
Every year, endocrinologists decide to retire when they reach a certain age, arguably, when they are still in their prime and benefit from significant clinical experience. Many would like to continue to serve, heal, care and share what they know, and they have the bonus of perspective.
Retirement indeed encourages perspective, and many physicians stepping outside the arena of a busy hospital or medical practice often feel a sense of unfinished business or, even worse, that they are no longer needed. They are so wrong – they can continue to contribute. Wisdom is a terrible thing to waste, doubly so when it can save lives.
How can retired doctors help patients with diabetes living in rural areas?
Patients with diabetes living in rural, underserved areas frequently experience less than adequate health outcomes, often exacerbated by higher rates of poverty, lack of health insurance and insufficient primary care and specialist providers. While this is a shocking situation, it is also an opportunity.
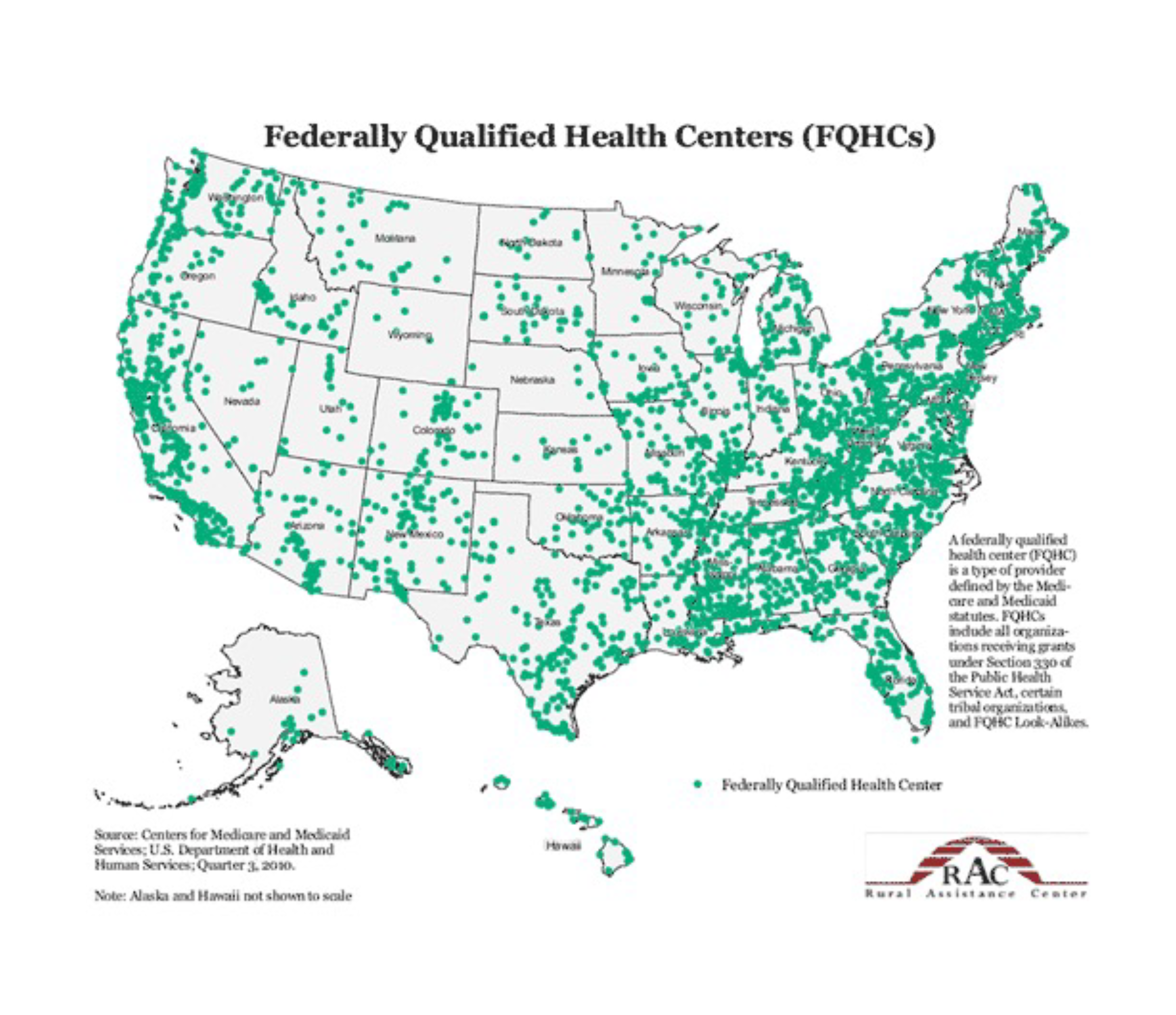
Many retired doctors are eager to offer their services and are looking for ways to reach out and help. At the same time, spread around the country are 1,400 Federally Qualified Community Health Centers (figure 1) that provide sorely needed medical services to patients, independently of their ability to pay. These centers, supported by $5.78 billion in U.S.- Federal funding, generally have skilled primary healthcare personnel, but many of them lack the ability to offer patients specialty care. Herein lies an opportunity to connect retired endocrinologists via telemedicine with patients attending these rural community health centers.
Can telemedicine help patients with diabetes?
How can this be done easily? The solution is telemedicine – for example, a doctor in Alabama would not have to leave home to help a person in an underserved rural community hundreds of miles away. Imagine that a primary care provider at a rural community health center refers a patient to an endocrinologist and provides detailed medical records and test results.
The endocrinologist then conducts an initial consultation with the patient via videoconference with the primary health care provider present; community health centers have the necessary technological infrastructure for such consultations. The endocrinologist then provides detailed recommendations regarding further laboratory assessment and patient management guidelines.
Follow-up sessions with the patient are arranged via telephone or, if necessary, videoconference to ensure they are on track with the ongoing care; in each case, they provide feedback to the primary healthcare provider. This helps build robust relationships with both the patient and provider – something most retirees miss the most about their medical careers.
How can this work without undue hassle? Providing detailed reports of the findings and recommendations can take time! However, various digital dictation software programs (such as Dragon Medical One) are available, which are highly accurate and secure. The endocrinologist can do the entire consultative process sitting at a home desk with a cup of coffee close at hand.
Perspective of a partially retired endocrinologist
Can this process work? Absolutely – Dr Richard Santen has been doing it for over six years. As a partially retired endocrinologist, he has managed to help treat people with diabetes in underserved rural areas in Southwest Virginia. He encourages other endocrinologists to follow in his footsteps with these comments:
“I’ve done much telemedicine-based diabetes management from the comfort of my study. In a way, technology has ‘rebooted’ my medical career. I am now encouraging other endocrinologists who have retired and are feeling the pangs of regret or are itching to ‘get back to work’ but still enjoy some of the benefits of retirement to take advantage of the remarkable advances in telemedicine to ‘reboot’ themselves and make a difference.”
Full disclosure – rebooting requires teamwork. You can’t just fire up your laptop and plug it into a medical ‘matrix.’ The staff at the rural community health centers play a pivotal role. They are, in essence, the management machine behind the whole process – they’re involved in scheduling, ordering medications and laboratory tests, non-urgent communications with patients, and coordinating consultations – rebooting can’t be done without their input and organizational muscle.
The “rebooting process” is also not entirely cost-free. It helps to have someone called a ‘navigator’ who can do the managerial component of the process: renewing the retired endocrinologist’s medical license, obtaining malpractice insurance, communicating with rural community health center administrators and building a relationship with them. Proprietary, secure dictation software is not free, but any cost incurred is an investment, and the return is worth it.
Dr Santen has found the whole process completely rewarding: all the benefits of providing specialized healthcare without the more burdensome aspects of running a medical practice. He comments: “I get to interact with patients, see a marked clinical improvement in them and be part of a team dedicated to caring. It has its challenges, but it’s medicine without the misery – no traveling, filling out endless forms, following someone else’s rigid regulations, chasing payments, and continually trying to squeeze more patients into shrinking appointment times.”
Retired endocrinologists re-entering practice
The last point is essential because time takes on a whole new meaning when one retires – one reflects on the extended period that was your career to date and knows that the time ahead of you is probably shorter. This usually means that one wants to make the most of it.
For some people, that may mean fishing or traveling, but for those who dedicate their lives to healing, it’s hard to close the door and walk away knowing there is still a significant need for your care. Nevertheless, limited time has a high value, so retired endocrinologists re-entering practice can decide how much they would like to spend. That could be as little as five hours a week or as many as twenty; that’s up to them. They cannot let demand determine their supply of time, or they will burn out.
Dr Santen comments that he knows of many specialists who have built highly successful careers and can now retire and enjoy the financial benefits of their hard work. They probably won’t miss the hassles of running a busy practice or the high-pressure demands of a big hospital. However, they will miss the patients and the immense satisfaction of caring and healing. It’s what made them want to be doctors. For them, telemedicine from their home provides a solution.”
References
- Rural Health Disparities, RHI hub. Rural Health Information Hub. Last Reviewed 11-28-2022 https://www.ruralhealthinfo.org/topics/rural-health-disparities
- Santen RJ, Nass R, Cunningham C, Horton C and Yei W, Intensive, telemedicine-based self-management program for rural, underserved patients with diabetes mellitus: Re- entry of retired endocrinologist into practice. Journal of Telemedicine and Telecare 2023 29(2): 153-161.
- Santen RJ Need for navigators for care of patients with diabetes in rural, underserved areas Trends Telemed E- Health 3(3), 2022.
- Santen RJ Re-entry of retired endocrinologists into practice: role of telemedicine for patients with diabetes in rural, financially underserved areas . Trends Telemed E-Health 3(2), 2022.
- Santen RJ “rebooting” after retirement: novel approach using telemedicine to solve the work-force gap in diabetes management Maturitas 133:68-69, 2020.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


