Professor Shaw-Ruey Lyu from Tzu-Chi University tells us how the discovery of the medial abrasion phenomenon, as a cause of knee osteoarthritis, has changed how it is best treated
The medial abrasion phenomenon (MAP) is an important cause of knee osteoarthritis (OA) that mainstream medicine has long neglected.
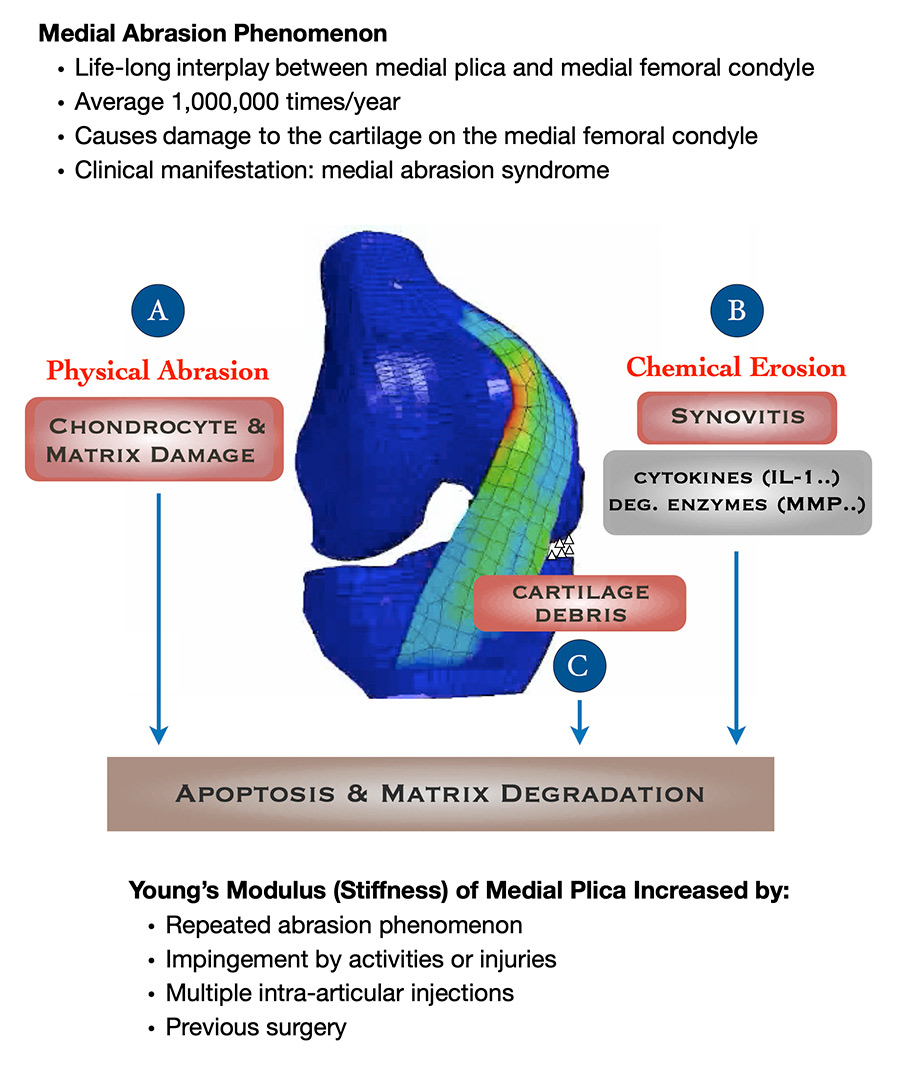
According to our series of studies, (1) the MAP can cause physical abrasion, which leads to cartilage debris and chemical erosions in the knee; all these factors then compound one another, making knee OA worse all the while. For example, more abrasion produces more cartilage debris which leads to more physical abrasion and synovitis (synovial inflammation); synovitis leads to biochemical erosion that further damages cartilage. A vicious circle ensues, and the patient suffers from worsening knee OA (Fig.1).
Why the knee health promotion option (KHPO) matters so much
For the last 25 years our practice has implemented the KHPO protocol (2) based on the discovery of MAP as an important cause of knee OA, and we have repeatedly seen that KHPO improves every aspect of the mainstream therapy for knee OA. In the following examples, smart knee care (SKC), (3) arthroscopic cartilage regeneration facilitating procedure (ACRFP), (4) high tibial osteotomy (HTO), unicompartmental knee arthroplasty (UKA, also known as partial knee replacement), and total knee arthroplasty (TKA) are some of the tools available in the KHPO protocol. Although also included in mainstream treatment for knee OA, HTO, UKA, and TKA under the KHPO are carried out with additional care to eliminate the MAP, which mainstream medicine doesn’t do.
Prevention and cure of knee OA is possible by SKC
If implemented in time, knee OA is not only preventable but also curable by SKC. SKC stops knee cartilage damage and facilitates its regeneration. Contrary to the common notion in mainstream medicine that worn cartilage cannot grow back, we have seen in our patient’s countless real-life re-growth of their worn-out cartilage just by SKC. Take a patient for example (Fig. 2):
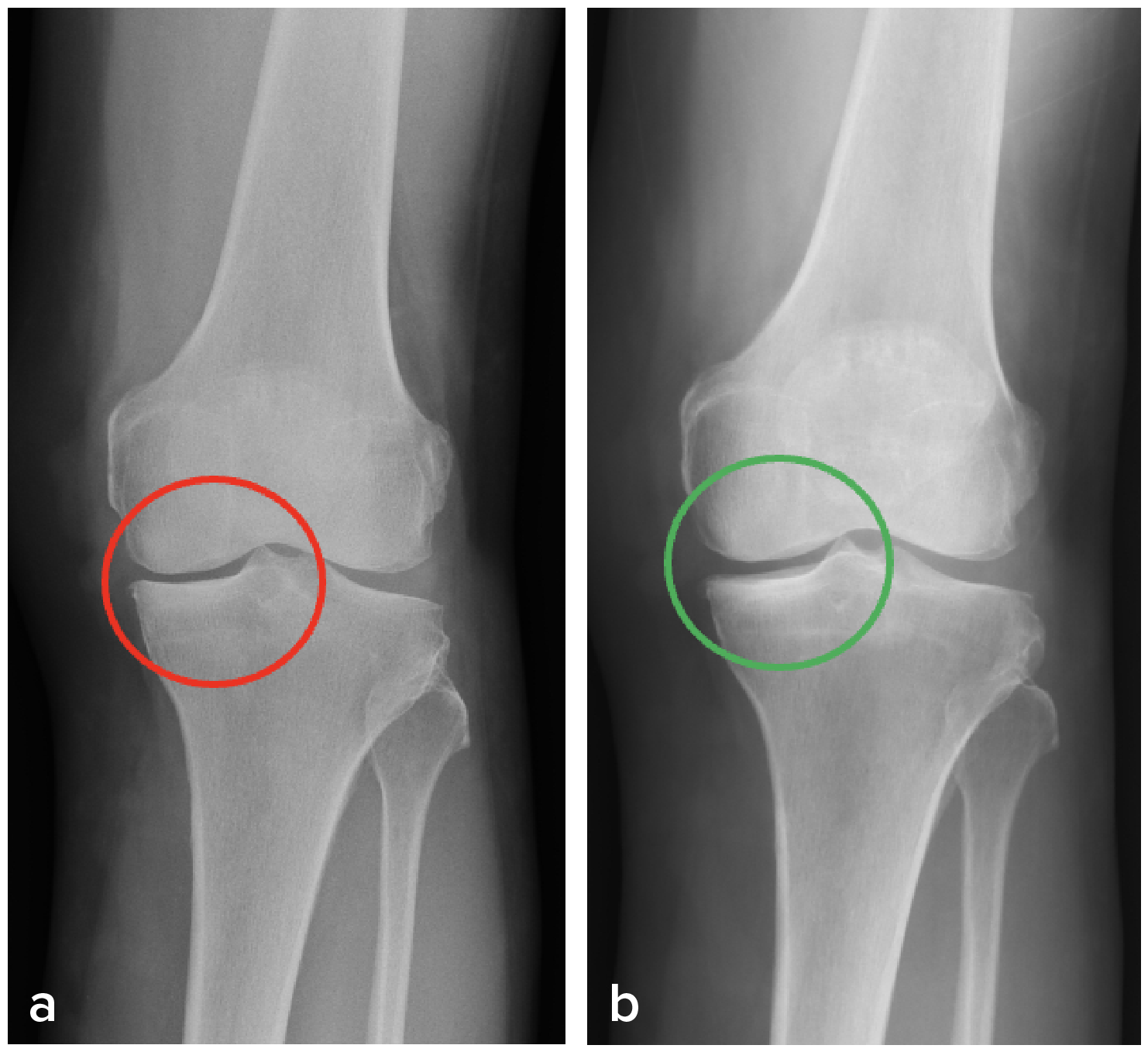
the radiographic manifestation could be observed in both his knees (b).
Reversal of natural course of knee OA is possible by ACRFP
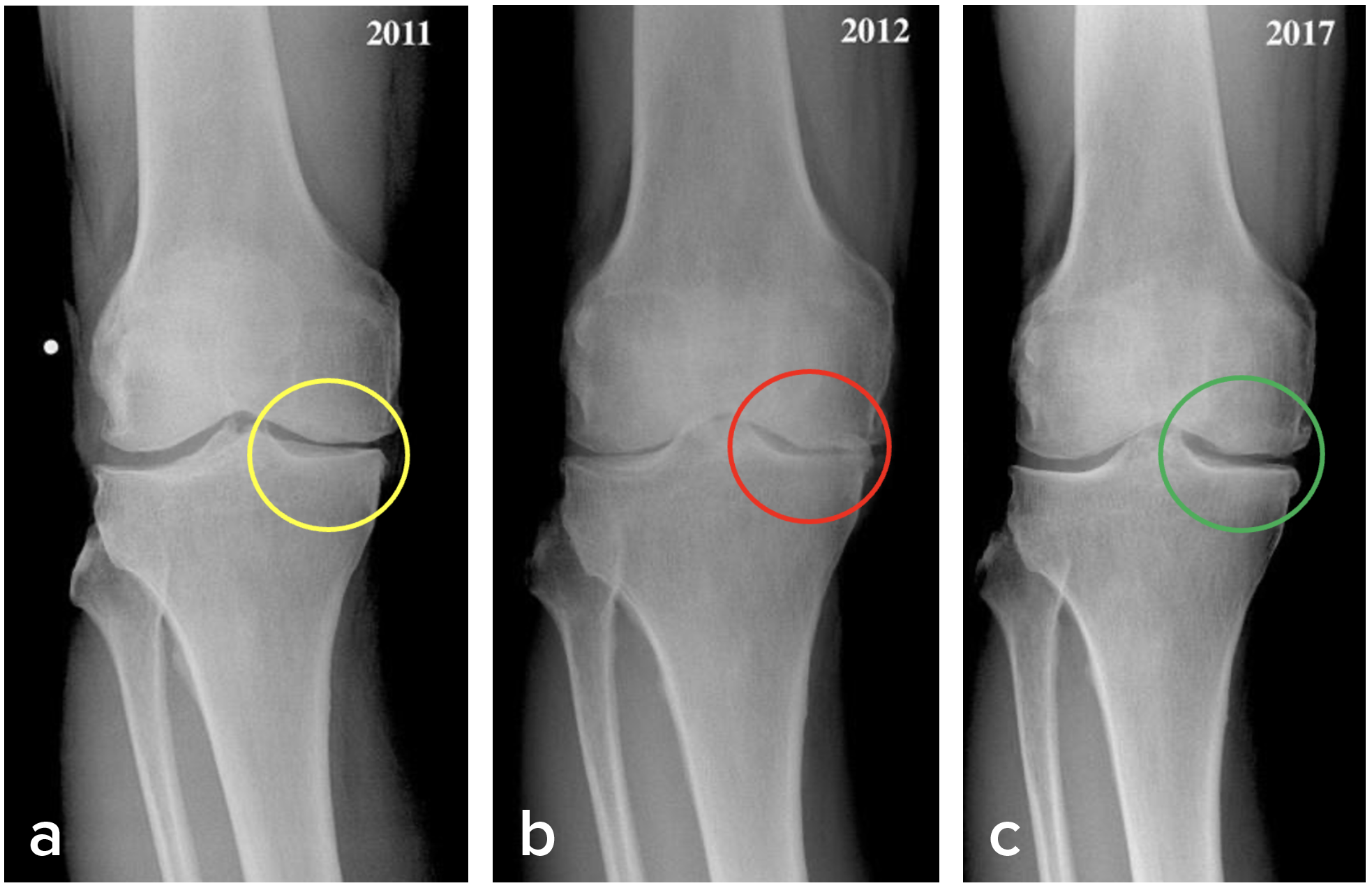
ACRFP removes the offending and abrasive medial plica and the sequalae of MAP, making the joint cavity a more hospitable space in which the damaged articular cartilage can grow back as 80% of ACRFP patients have demonstrated according to our clinical outcome studies. (4-7) Figure 3 shows an example of how ACRFP stops knee cartilage degeneration and facilitates its regeneration: a, AP standing view of a 69-year-old female patient having stage III OA over the medial compartment of her right knee; b, after one year of conservative treatment, the condition deteriorated; c. 5 years after ACRFP, X-ray images show obvious improvements in her knee.
Elimination of MAP could improve the outcome of traditional knee OA surgeries
It is worth pointing out again that although also included in mainstream treatment for knee OA, HTO, UKA, and TKA under the KHPO are carried out with an additional goal of eliminating the MAP. The outcome of mainstream surgery (HTO, UKA and TKA) could be improved under the KHPO because they are performed concomitantly to eliminate the MAP.
ACRFP could improve the outcome of HTO
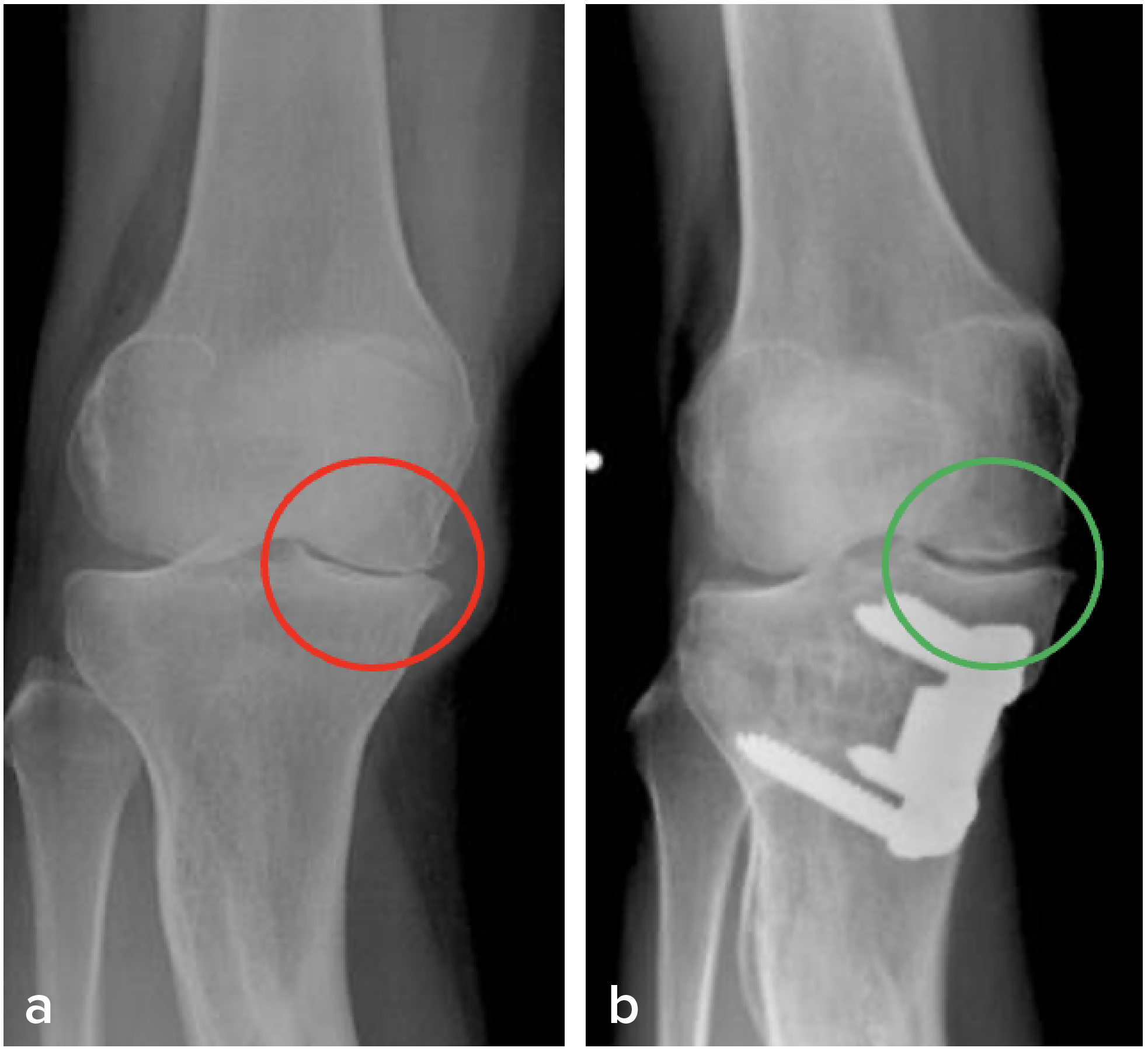
HTO is nowadays regarded more as a buying-time procedure before TKA. But that grim prospect brightens up when HTO is performed concomitantly with ACRFP. Our patients who received HTO and ACRFP together have enjoyed good long-term results as shown in Figure 4, which is an example of the reversal of the degeneration process after receiving ACRFP and HTO: a, AP standing view of a 45-year-old female patient having stage IV traumatic OA over the medial compartment of her right knee; b, 10 years later, an X-ray image shows obvious cartilage regeneration.
The elimination of MAP also improves the outcome of knee arthroplasties
Persistent post-operative pain (PPOP) has been a common occurrence in about 10 to 53% of patients after arthroplasties and is associated with reduced health-related quality of life. However, by performing UKAs or TKAs that also eliminated MAP, we could satisfy nearly 100% of patients do not suffer from PPOP. (8)
KHPO and cell therapy is a perfect combination for knee OA treatment
KHPO alone has brought about cartilage repair and regeneration in about 80% of patients after ACRFP. (4-7) Cell therapy could be an add-on for stages I-II patients when doing SKC. For patients receiving ACRFP, adipose tissue could be obtained during ACRFP. The timeline of this stem cell therapy process dovetails very nicely with the timeline of recovery of a typical KHPO-treated patient, making the KHPO/cell therapy a perfect combination for treating knee OA. (2)
We have discovered evidence that the MAP contributes to the pathogenesis of knee OA. Identifying MAP and early intervention using SKC and ACRFP can prevent further degradation of cartilage and improve quality of life. Even in later stages of knee OA, ACRFP could prevent the need for the implantation of prosthesis and enable many patients to keep their natural knees. Moreover, the outcome of mainstream surgery (HTO, UKA and TKA) for knee OA could be improved under the KHPO because they are performed concomitantly to eliminate the MAP. Based on the experience gained from our clinical encounters and research, we have put forward the notion of the KHPO as a suggested protocol for the comprehensive treatment for knee OA. Our discovery and proposed interventions (SKC, ACRFP, add-on cell therapy, and concomitant removal of MAP when performing osteotomy or arthroplasties) are justified to be included in the clinical treatment of knee OA.
Acknowledgment: Publication of the present article was supported by the BIONET Corp.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


