Chronic wounds are a significant burden to patients and health systems; Manuela Martins-Green from the University of California tells us how her research in understanding the dynamics of wound healing could aid new approaches to wound care
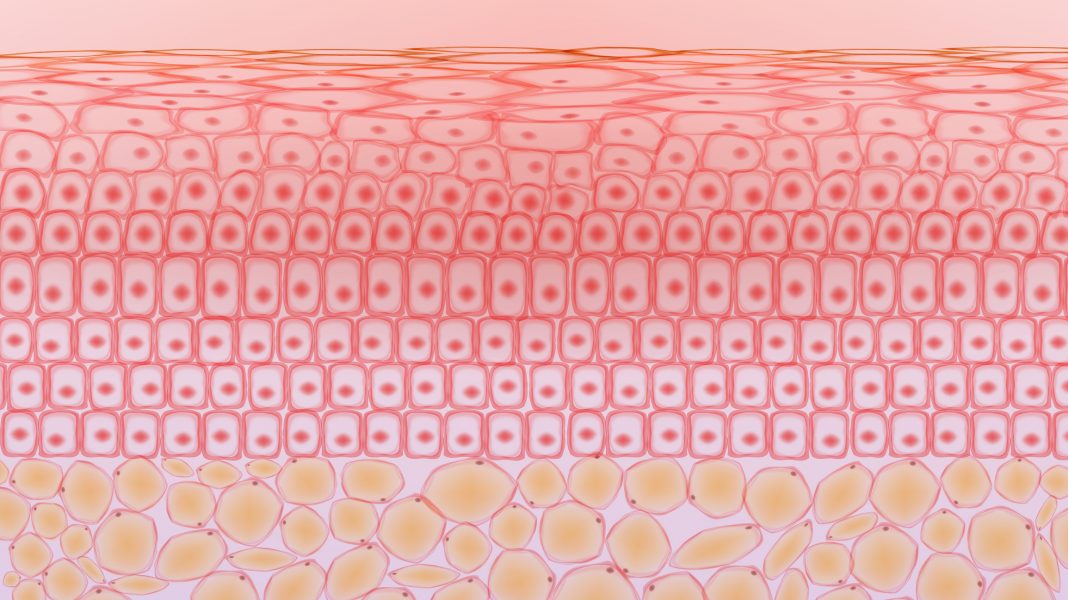
The skin is the largest organ in the human body. It is the barrier that protects the organs from the environment, functioning as an interface between the environment and the inside of the body. Residing on the skin is a complex and diverse community of microbes called the microbiome.
Trillions of microbes across bacterial and fungal families use a wide range of aerobic and anaerobic metabolic pathways to survive. Considerable effort is being put into studying the role of the microbiome in skin infections, disorders, and disease. Host-microbiome interactions are particularly important during wound healing because changes in microenvironmental conditions in the tissue can change commensal bacteria into pathogens that infect the wound chronically, including forming biofilm.
The healing of cutaneous wounds
Healing of cutaneous wounds (wounds of the skin) occurs by a series of processes that follow an orderly path both in space and in time. In normal wound healing, there are four sequential phases that contribute to the rebuilding of the damaged tissue and closure of the wound: Hemostasis (stopping of the bleeding), inflammation (when leukocytes come to the wound to remove pathogens and secrete molecules that stimulate the next phase of healing), proliferation (when the cells of the tissue, primarily fibroblasts, repair the damaged tissue, endothelial cells form microvessels, and keratinocytes close the wound) and remodeling (when excess tissue is removed by specialized cells).
Chronic wounds fail to follow this progression in time and/or space, get staled at the inflammatory phase, and do not repair.
The skin’s complex microbiome is also important for the healing process. Indeed, cutaneous wound healing results from the interaction between the host component and the microbiome in the skin. It is thought that for the healing to occur normally, the wound needs to be populated with 105 bacteria per gram of tissue.
These microbes are important for attracting neutrophils, a type of white blood cell that cleans the wound of pathogens, but also produces molecules that trigger the next wave of leukocytes – the monocytes, which mature into macrophages in the wound tissue. Such macrophages are very important for triggering the repair phase of healing and progression of the wound toward closure.
Wound colonization with the skin microbiome
The progression from wound colonization with the skin microbiome for normal healing to infection leading to chronicity, depends not only on the bacteria count, the species present, and their virulence but also on the levels of oxidative stress (OS) in the wound tissue. Indeed, we have recently shown that increased OS levels in the wound correlate with increased chronicity.
Moreover, without high levels of OS, biofilm taken from chronic wounds and placed in new excision wounds do not create chronic wounds. Similarly, high levels of OS in the wound tissue, in the absence of the skin microbiome, do not lead to chronic wounds. Therefore, high levels of OS in the wound and the microbiome are critical for biofilm formation and chronic wound development.
Approximately ~80% of chronic wounds contain biofilm, whereas only ~6% of acute wounds contain biofilm. There is increasing evidence that bacteria in chronic wounds live as communities within the biofilm. Bacterial biofilms are bacteria cells embedded within an exopolymeric matrix composed of DNA, RNA, proteins, and polysaccharides. When within this matrix, the bacteria become protected from host defenses and tolerant to antibiotic treatments. One of the current ways to treat chronic wounds with biofilm is by debridement, which removes both the bacteria and exopolymeric substance that the bacteria are embedded in.
However, during debridement, not all bacteria are removed; some of the bacteria that are buried deep in the wound tissue remain and will return as biofilm within 72 hours after debridement, even with treatment with antibiotics/antimicrobials and more classic chronic wound treatments.
New chronic wound treatments
To find new treatments, we have developed a model of chronic wounds in diabetic mice that mimics many of the characteristics of chronic wounds in diabetic people. Using this model, we set out to understand how biofilm develops from its inception until its maturity. If we understand the dynamics of biofilm development, we might be able to develop ways to dismantle it in chronic wounds.
For this, we sequenced the bacterial species of the wound from wound initiation to fully chronic wounds, something that is not possible in humans because wounds presented to clinicians are already fully chronic.
We looked for indicator species to determine which bacterial species were strongly associated with healing wounds where OS levels are low or associated with chronic wounds where OS levels are very high. We found that healing wounds were colonized by a diverse and dynamic bacterial microbiome that never developed biofilms, even though biofilm-forming bacteria were present. In contrast, chronic wounds had low bacterial diversity.
They were colonized by several clinically relevant, biofilm-forming bacteria such as Pseudomonas aeruginosa, Enterobacter cloacae, Staphylococcus xylosus, Corynebacterium frankenforstense, and Acinetobacter sp. These findings show that high levels of OS in the wound significantly altered the bacterial wound microbiome, decreasing diversity and promoting the colonization of bacteria from the skin microbiome that can form biofilm.
Our studies of the bacterial microbiome through time in chronic wounds of mice suggest that a critical point of treatment to prevent the return of the infection/biofilm would be right after debridement. Indeed, many treatments have been used over time after debridement of wounds, including nanocrystalline silver, sustained release iodine, and topical application of antibiotics/antimicrobials.
Although these small molecules should be successful treatment options because they have low cytotoxicity, can be applied topically, are inexpensive, and off the shelf, these treatments are frequently ineffective, and the bacteria and biofilm return. Therefore, new approaches are needed.
Killing bacteria within the tissue of chronic wounds
We have recently shown that sodium chlorate is very effective in killing anaerobic bacteria found deep in the tissue of chronic wounds. Some anaerobic bacteria typically use nitrate reductase (Nar) to reduce nitrate to nitrite and survive in low-oxygen environments. However, this enzyme can also reduce chlorate to chlorite, a toxic oxidizing agent.
Therefore, chlorate can be used to specifically eradicate hypoxic/anoxic nitrate-respiring bacteria, which are generally tolerant to conventional antibiotic treatments. Moreover, our studies also show that N-Acetyl cysteine (NAC) at a pH below the pka is very effective in killing bacteria by inhibiting protein synthesis (which is critical for bacterial cell division) and breaking down biofilm. Treatment with chlorate and NAC, which is also an antioxidant molecule, could not only kill the bacteria and dismantle the biofilm but also help recover the host tissue by decreasing the levels of OS.
This outcome may put the wound on a course to healing and receptive to treatments that help in the generation of the healing tissue and closure of the wounds.
Therefore, small, stable molecules that survive the harsh environment of chronic wounds and are specific for treating biofilm without adversely affecting the host tissue are viable treatments for chronic wounds with biofilm. At the same time, they should be available off the shelf and affordable, allowing for low healthcare costs.
This approach can be successful because these molecules will be inhibiting processes that are critical for chronic wound initiation, i.e., high OS and biofilm formation, and have been used in humans before. In addition, our approach will allow for subsequent successful treatments using matrices containing growth factors, angiogenic factors, and protease inhibitors to facilitate wound tissue repair and closure.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.