Concerted efforts are needed to close knowledge gaps around mpox to improve preparedness and response efforts for this neglected disease
Mpox, formerly known as monkeypox, is a previously neglected re-emerging zoonotic disease caused by monkeypox virus (MPV), genus Orthopoxvirus, family Poxviridae. This virus can cause severe illness in infected patients and is endemic in numerous countries across Central and West Africa, including the Democratic Republic of Congo (DRC), Nigeria, Cameroon, Sierra Leone, Ghana, Liberia, and others.
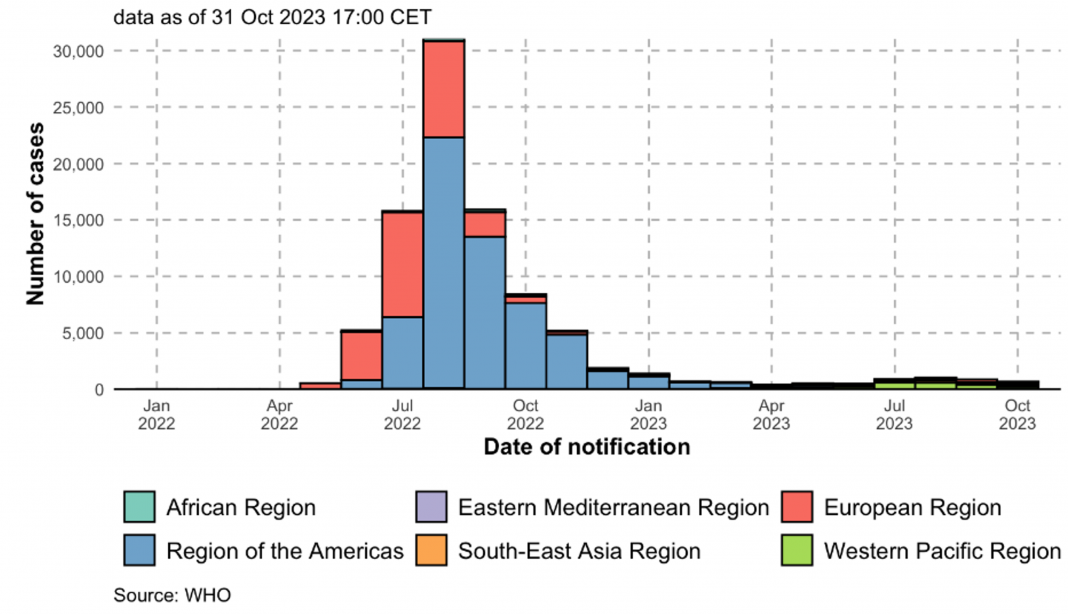
However, in 2022, a global mpox outbreak led to the declaration of a public health emergency of international concern by the World Health Organization, with more than 90,000 confirmed cases reported from non-endemic global regions. While swift responses to this outbreak helped reduce case trends across highly impacted regions by Fall 2022, including the distribution of vaccine and therapeutics to at-risk communities, as well as increased public awareness, ongoing outbreaks in endemic regions continue to have deleterious effects on public health.
A short history of MPV
MPV was first identified in 1958 among captive non-human primates in Denmark, with subsequent identification of suspected or confirmed cases among multiple captive animal species in additional countries over the following decade. The first human mpox cases were not identified until 1970 in the Democratic Republic of the Congo.
There are two distinct clades of MPV: Clade I, which is endemic in regions of Central Africa; and Clade II, which is in regions of West Africa. Clade II MPV has been further subdivided into two subclades: clades IIa and IIb, with Clade IIb being responsible for the global mpox outbreak.
Clade I MPV infections are associated with more severe disease, with case fatality rates having ranged from 1- 10%. It should be appreciated that poor disease outcomes may also be influenced by healthcare access and social determinants of health. However, these fatality rates may also be influenced by limited identification of mild disease cases due to lack of diagnostic access or ongoing surveillance programmes.
While there have been numerous observations regarding MPV infections in animals from prior serological surveillance studies and laboratory investigations, there is a paucity of knowledge regarding the susceptibility of animals in non-endemic regions, including wild, captive, agricultural and domesticated animals. The reservoir for the virus, as well as potential intermediate species, are largely unknown, though rodent species are regarded as the most likely reservoir.
During the 2022 global mpox outbreak, Clade IIb infections were associated with atypical clinical presentation. Historical “smallpox-like disease” presentation of mpox with lesions concentrated on the arms, legs, hands, feet, face and trunk with all lesions in the same stage of development (synchronous).
Further, Clade IIb infections during the global outbreak were strongly associated with sexual contact between gay, bisexual and other men who have sex with men (GBMSM) (95.2% of all reported cases globally). HIV positivity was also found to be associated with Clade IIb infection; however, it is unknown whether there is an underlying causal association.
While these trends suggest that Clade IIb differs substantially in its epidemiology from other MPV clades, there are limitations in our current knowledge. For example, the atypical lesion presentation resulting from Clade IIb infections may result in misdiagnoses, including other sexually transmitted infections. There are also knowledge gaps regarding virus transmission during sexual contact or intercourse.
Additionally, ongoing stigma encountered by GBMSM communities may have impacted reporting of sexual contact-associated mpox cases for Clade I and Clade IIa virus. While our recent identification of Clade I- associated mpox via sexual contact demonstrates that this mode of transmission is not limited to Clade IIb MPV, there is little information on how the frequency of these events.
MPV transmission
MPXV transmission has primarily been regarded to occur through close contact and mitigated by saliva and/or respiratory secretions from infected patients or through contact with exudate or crust material from lesions. Viral shedding in faeces has been observed in experimentally infected prairie dogs; however, the implications of this for virus transmission in humans is unknown. Early mpox outbreaks were largely considered to result from animal-to-human transmission events (zoonosis) and the risks of sustained human-to-human transmission were considered to be very low.
However, there have been increasing trends of human-to-human transmission in recent years, including during the global mpox epidemic, as well as the re-emergence of mpox in Nigeria during the 2017-2018 outbreak.
Ongoing mpox priorities
Considering the recent global mpox outbreak and ongoing outbreaks in endemic regions of Africa, there has been renewed focus on identifying mpox research priorities. These were highlighted in a recent global WHO R&D Blueprint meeting and included the needs for increased surveillance and response capacity that includes endemic and non-endemic regions. Further, increased considerations for social determinants of health, as well as integration of community-led initiatives should be undertaken.
There is a critical need to address mpox knowledge gaps, including the over- representation of cases among social groups, and infection risks and severities based on transmission routes and exposure settings. Given these epidemiological differences, and the phylogenetic differences identified between the MPXV clades, comparative analysis of viral characteristics, pathogenesis and countermeasure efficacies between isolates from the global outbreak and previously characterised clades needs to be undertaken.
- Increased prioritisation of collaborative research and clinical partnerships with regional partners in mpox endemic regions.
- Enhanced surveillance and response capacities in endemic areas.
- Increased integration of community engagement and partnerships in mpox preparedness and response efforts.
More than half a century following the first identification of human mpox, concerns regarding the global threat of this disease were quickly replaced with the reality of a historic global outbreak. However, the expansive coverage and reporting on mpox quickly receded as cases dropped precipitously in Fall 2022. This contrasts with the ongoing impacts of mpox in endemic regions, including those being seen now in the Democratic Republic of the Congo.
Further, while the health and economic impacts of human MPX in endemic regions of West and Central Africa have been well documented, there has been limited international investment in sustainable preparedness and response efforts. Thus, while the recent global mpox outbreak garnered international spotlight and renewed interest in this virus, threat reduction for this neglected disease requires concerted efforts for sustained control efforts in endemic regions.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.