Richard J. Santen, MD, Emeritus Professor of Medicine at the University of Virginia in Charlottesville, Virginia, USA, delineates the characteristics of patients with diabetes residing in rural underserved areas, including the role of meal replacements for weight loss
Patients with diabetes residing in rural, economically challenged and medically underserved areas generally lack endocrinologists for consultative evaluation and management. (1,2) One solution to the problem is recruiting retired endocrinologists to care for these patients by telemedicine. This can be facilitated by partnering with rural community health clinics.
In the United States, a Federal program funds 1,400 rural clinics and supports the providers and clinical educators to instruct patients regarding diabetes mellitus management, nutrition, laboratory testing, and radiology.
My experience over the last six years as a partially retired endocrinologist indicates that such a program is beneficial and results in lowering the hemoglobin A1c levels in patients with diabetes (3).
Nutrisystem D meal replacement diets
However, a major drawback has been the inability of patients to lose weight, even with intensive counseling and encouragement. In these rural areas, the level of education is less than in urban areas and access to healthy, low-calorie-density food is limited.
Most patients evaluated in my program had marked obesity with an average weight of 226±60 pounds (103 kg). (3) As control of obesity is now considered by professional organizations a goal equal to glucose management for patients with diabetes, a solution to achieving weight reduction was critically needed.
In a eureka moment, a practical solution became apparent. The veterinarian taking care of my dog with diabetes advised me to cut down her food intake by one-half bowl a day. The dog’s insulin requirement decreased substantially, as did her glucose levels.
This generated the idea that the use of meal replacements delivered to my patients’ homes might be a way to encourage a reduction of calories and resultant weight loss. (4) To test this hypothesis, we conducted a pilot trial utilizing the Nutrisystem D meal replacement diets in patients living in rural areas. (5)
The Nutrisystem D system (5) allows patients to choose the dietary elements they want while strictly maintaining the calorie content and composition. These diets consist of an average of 1,450 to 1,550 kilo-cal/day for men and 1,200 – 1,250 kilo-cal/day for women. The plan includes Nutrisystem breakfast, lunches, dinners and two snacks for male patients and one for females. These diets provide a balanced diet with 45 to 50% carbohydrates, 20 to 30% protein, and less than 30% total fat. Food is shipped to the patients’ homes monthly.
A continuous glucose monitoring (CGM) system
Because we anticipated that hypoglycemia might occur acutely upon using this diet, the patients were given a continuous glucose monitoring (CGM) system during the first ten
days of the study. In the first patient entered, hourly glucose levels, which were monitored every five minutes, fell rapidly from 220 to 85 mg per cent on the first day of the study.
In response to this, the insulin dose was lowered by 50% from baseline values in this patient and then routinely and in all subsequent patients. After that, episodes of very low glucose (i.e., less than 54 mg per cent) occurred in only two of 11 patients and low values (i.e., 54 to 69 mg per cent) in five of 11.
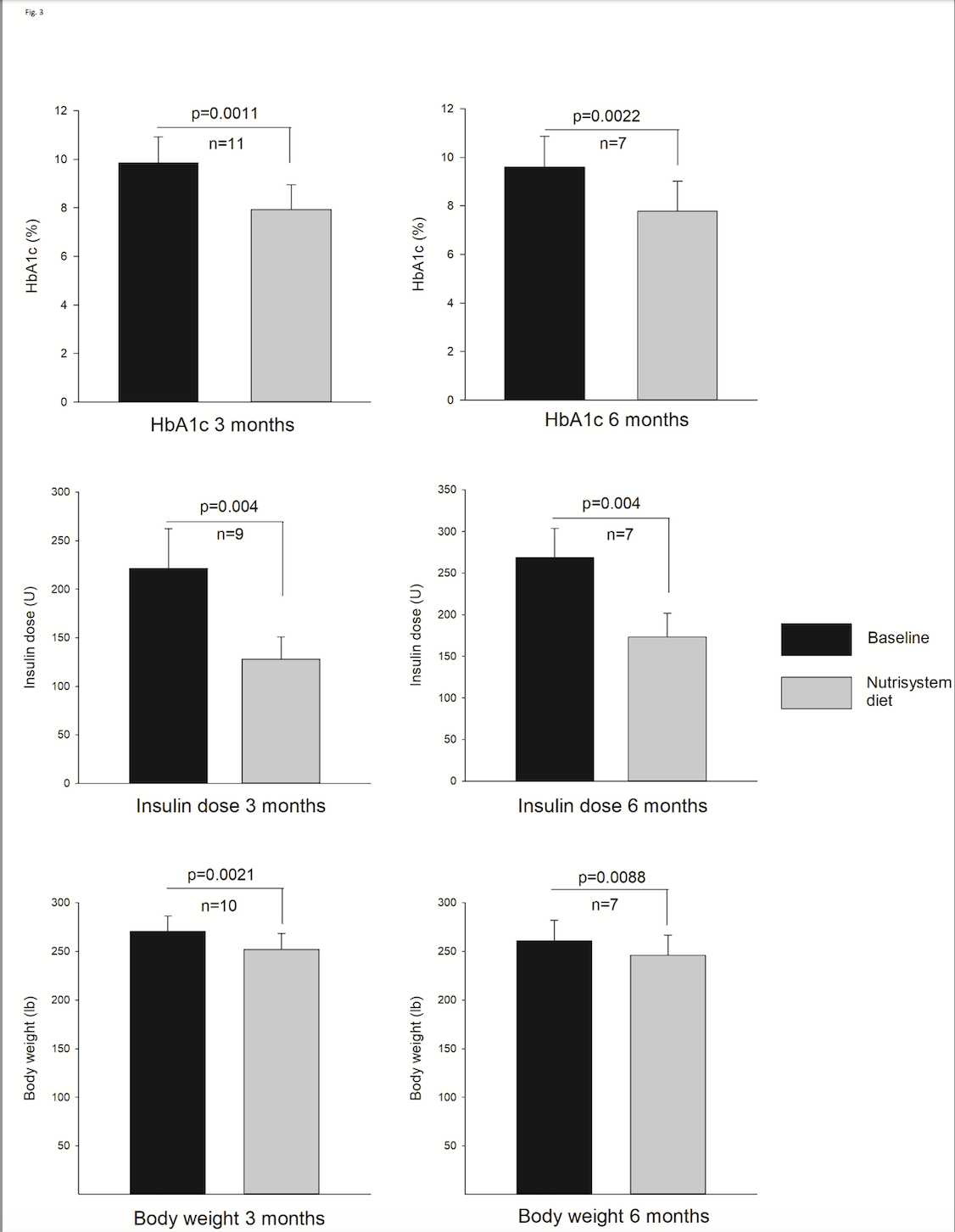
The objective of attaining statistically significant weight loss has been accomplished. In the 11 patients evaluated at the three-month mark, a reduction in body weight of 7.1% was observed (see figure) and persisted in the seven patients completing the study. During the entire course of the study, insulin doses were recommended according to an algorithm incorporated in a program called Glucomander-outpatient, a commercial product of the Glytec Company (6).
Following the weekly insulin reductions, as shown in the figure, the baseline hemoglobin A1c levels fell significantly. In the 11 patients completing the three-month protocol, the hemoglobin A1c level decreased from 9.85±0.33% at baseline to 7.93±0.31% SEM (P equals 0.004). In individuals who completed the entire six-month duration, the levels reduced from 9.60±0.49% at baseline to 7.7±0.47% SEM (P equals 0.004). Lipid levels did not change significantly when comparing the baseline with three months.
Can a meal replacement system result in weight loss?
Our prior study, encompassing 139 patients, showed substantial improvement in glycemic control, but, importantly, there was no statistically significant reduction in weight. (3) The current pilot study was designed to test whether a commercial meal replacement system could result in weight loss, and this was accomplished. Compliance was highly variable and seemed likely to influence both body weight and insulin levels. We tracked the level of compliance in following the diet during the entire six months, and there was a trend toward downward compliance from 8.85 on a scale of 0-10 to a level of 7.66.
The actual purpose of meal replacements was to teach patients the value of reduced calorie intake and a balanced diet in lowering their glucose levels. I think this is a superior method to instruct about diet than the usual didactic method using food samples to illustrate the quantities and types of food to be ingested. Patients commented that they learned about diet by seeing what foods were delivered to them in monthly shipments.
Glucose control of patients with diabetes in rural areas
Improving the glucose control of patients with diabetes in rural, financially challenged, underserved areas is difficult and requires a team effort of providers, nurse educators, and specialists. Even then, success is frequently limited by the ability of patients to follow an appropriate diet.
My conclusion from using meal replacements is that these are excellent educational tools to teach patients the value of caloric restriction and careful dietary monitoring. This study provided substantial evidence of the importance of meal replacements in improving the care of patients with diabetes in underserved rural areas. This concept now requires confirmation and a large, randomized control trial to determine if this approach is superior to usual care.
References
- Bell RA, Quandt SA, Arcury TA, Snively BM, Stafford JM, Smith SL, Skelly AH. Primary and specialty medical care among ethnically diverse, older rural adults with type 2 diabetes: the ELDER Diabetes Study. Journal of Rural Health. 2005;21(3):198-205.
- Ross SR, BSN, ARNP, Benavides-Vaello SP, MPAff.BSN, RN, Schumann LP, Haberman MP. Issues that impact type-2 diabetes self-management in rural communities. [Review]. Journal of the American Association of Nurse Practitioners. 2015;27(11):653-660.
- Santen RJ, Nass R, Cunningham C, Horton C, Yue W. Intensive, telemedicine-based, self-management program for rural, underserved patients with diabetes mellitus: Re-entry of retired endocrinologists into practice. Journal of Telemedicine & Telecare.29(2):153-161.
- Kempf K, Rohling M, Niedermeier K, Gartner B, Martin S. Individualized Meal Replacement Therapy Improves Clinically Relevant Long-Term Glycemic Control in Poorly Controlled Type 2 Diabetes Patients. Nutrients. 2018;10(8):2018.
- Santen RJ C, Horton C, Nass R, Yue w. Meal replacements in conjunction with an integrated, technology-driven strategy for treatment of patients with diabetes in rural, underserved areas: a pilot study Trends Telemed E-health. 2023;4(1):1-4.
- Bode B CJ. Glucomander outpatient, a cloud-based management solution, titrated patients to goal in 11 days and sustained a 2.6% drop in HbA1C over 6 months. American Diabetes Association Abstract 2017.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


