Photodynamic therapy, using visible light with lower energy, causes fewer side effects when treating cancer, find Drs. Mary Potasek, Evgueni Parilov, and Karl Beeson, Co-founders of Simphotek, Inc
You are probably familiar with x-ray radiation therapy for treating cancer. But do you know that x-rays are ionizing radiation that can cause damage to many tissues besides killing cancer cells? Simphotek and others are using near-infrared or “gentle” visible light whose wavelength is longer than x-rays and with much lower energy so that it causes fewer side effects.
The novel therapeutic modality known as Photodynamic Therapy (PDT) can do just this. PDT does not cause nausea as chemotherapy does, does not damage ordinary tissue as x-ray radiation does, nor does it require removing or damaging parts of the body as surgery does.
A new approach for killing cancer with light: photodynamic therapy
PDT uses light (usually provided by a laser), a light-sensitive drug and molecular oxygen to trigger multiple cascading events that generate a cytotoxic agent, singlet oxygen, that kills cancer cells. There are various forms of PDT treatment including External Beam or surface (EB-PDT), Intracavity or intraoperative (icavPDT), and interstitial (I-PDT). The first method is used mainly for skin conditions and cancers where the drug is applied superficially, and the treated area is exposed to light. The icav-PDT is usually performed after a surgical procedure, such as lung surgery, where a cavity is either present or formed by the surgery.
A photosensitive drug is administered into the body and is “activated” by the treatment laser light. I-PDT is used to treat solid cancers that are deeper in the body, such as the brain, esophagus, bladder, head and neck, cholangiocarcinoma, lung, and prostate. Light travels only a few millimeters in tissue so another mechanism must be added for successful treatment. These treatments use cylindrical diffusing optical fibers that tunnel the light from external lasers directly into the tumors and uniformly distribute it in the cancerous areas.
The amount of the delivered visible light matters
The amount of the delivered visible light matters, as it should be above a therapeutic threshold established by previous and current clinical trials. Because it is practically impossible to perform measurements everywhere inside the tumor to make sure that the light dose is delivered correctly, computer simulations based on advanced mathematical models of light propagation in human tissue are performed before the treatment starts. The EB-PDT can be done without extensive mathematical simulations, but the last two types of photodynamic therapy require advanced mathematical simulations to determine if the prescribed amount of light is delivered to various sections of the tumor, such that it is sufficient to kill cancer cells.
Simphotek has been supported by the United States National Institute of Health (NIH) to create such a simulation research tool for solid cancers and it’s called Dosie™.
Simulating Cancer Treatment with Dosie
There are several simulation methods that can model certain aspects of the photodynamic therapy process, but they do not cover everything that is needed for complete cancer treatment simulation. To the best of our knowledge, Dosie is the first comprehensive tool to simulate the PDT process including the light transport, drug, and molecular oxygen interactions to create the cytotoxic agent, singlet oxygen, which kills cancer. Treating cancer is complex and just as for radiation therapy, it requires advanced computer simulations.
Treating cancer with light requires advanced computer simulations
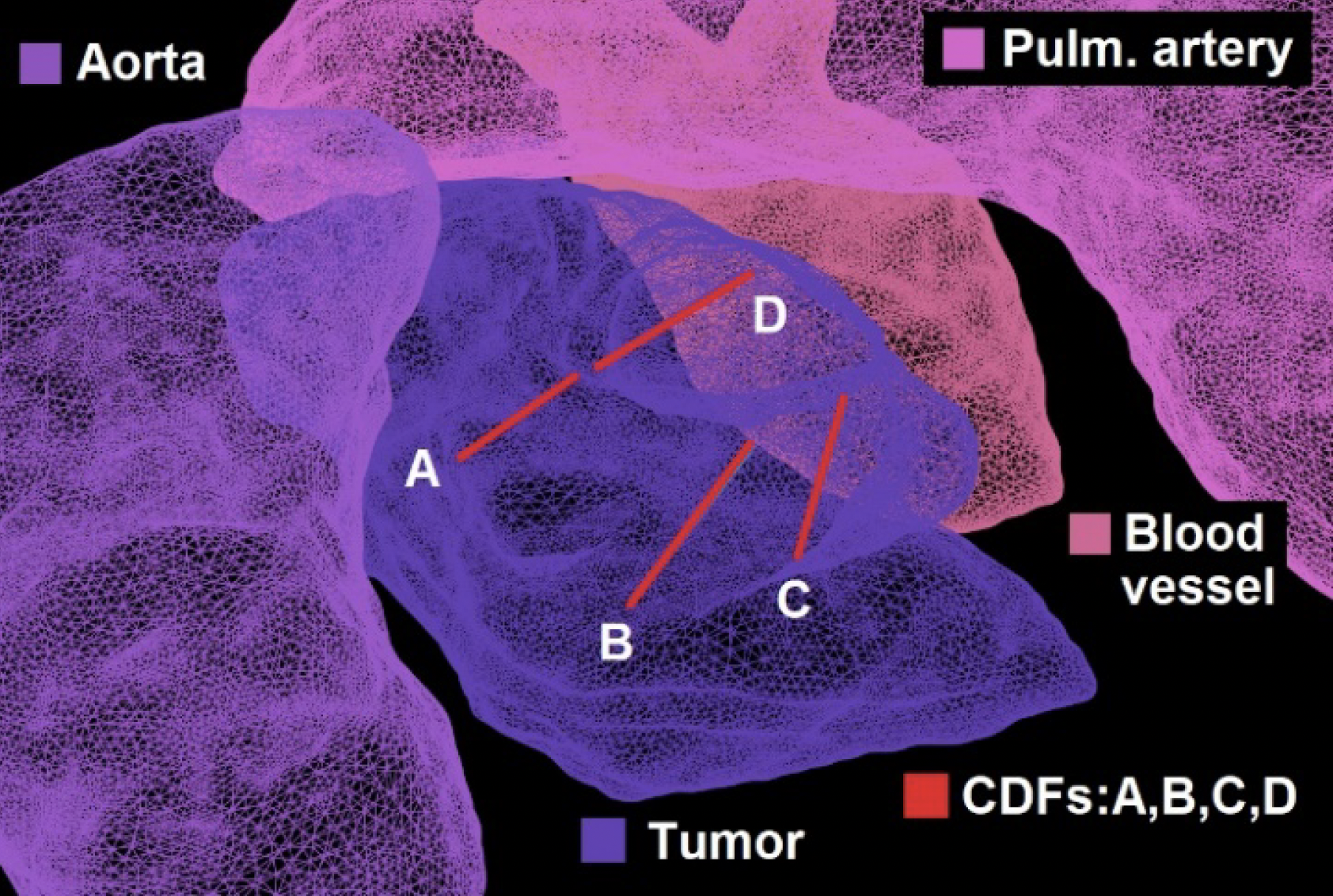
Starting with a CT scan or MRI of the tumor, a detailed 3D model of the tumor and its surroundings is created. Using state-of-the-art 3D graphics, Dosie can guide the physician in near real-time during the icav-PDT or I-PDT treatment to visualize the portion of the tumor that receives a therapeutic visible light dose to ensure a uniform light delivery. One of the benefits of using Dosie is its ability to estimate not only the conventional light dose but also the state-of-the-art PDT dose (that includes the variation of the drug concentration in the tumor) and singlet-oxygen dose (that estimates the amount of the cancer-killing agent and its distribution). The most common type of PDT is EB-PDT, which is responsible for most of the global PDT market. The total market is anticipated to reach more than USD 15.1 Billion by the end of 2031 and is projected to advance at a CAGR of 13.5% from 2022 to 2031 (1).
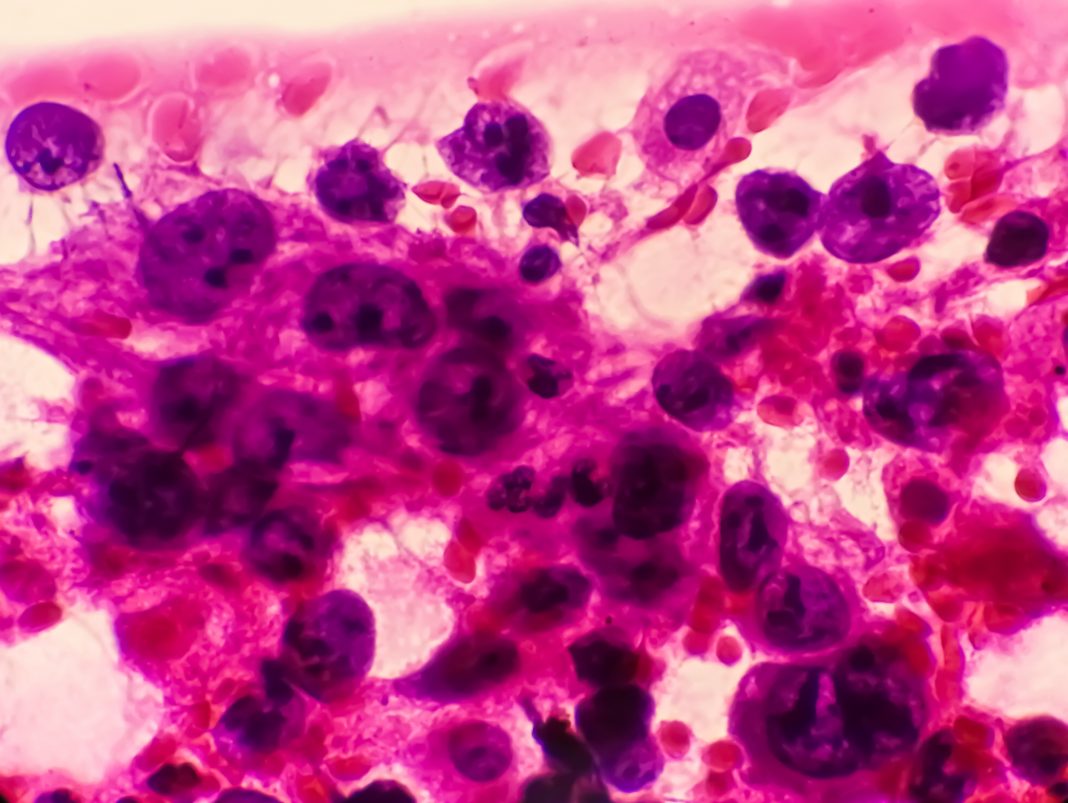
North America is expected to dominate the photodynamic therapy market, due to a high rate of adoption and new product launches by market players (2). Simphotek and its academic collaborators have treated a number of different cancers but the most recent one is non- small cell lung cancer that manifests itself as an endobronchial tumor growth near or inside the airway. Unfortunately, the tumor can become large enough to block the bronchus and in doing so it also becomes intertwined with several other tissues including blood vessels. The mixture of different tissues makes treatment planning difficult.
North America is expected to dominate the photodynamic therapy market, due to a high rate of adoption and new product launches by market players (2). Simphotek and its academic collaborators have treated a number of different cancers but the most recent one is non-small cell lung cancer that manifests itself as an endobronchial tumor growth near or inside the airway. Unfortunately, the tumor can become large enough to block the bronchus and in doing so it also becomes intertwined with several other tissues including blood vessels. The mixture of different tissues makes treatment planning difficult.
Image Guided I-PDT Treatment for MCAO
Malignant central airway obstruction (MCAO) is becoming a serious problem for patients with lung cancer. Lung cancer is the most common cancer and the leading cause of death in both men and women (3). The American Cancer Society estimates that for 2023 there will be about 238,340 cases of lung cancer (67,160 in men and 59.910 in women) in the United States (3).
Global lung cancer market revenue was worth USD 21.1 billion in 2021, growing to USD 67.9 billion by 2030 with a 14.1% CAGR from 2022 to 2030. North America has dominated with more than 35.5% of lung cancer market share in 2021 (4). Lung cancer is often treated by radiation and chemotherapy both of which can lead to damaging effects on non-cancerous tissue. Applying PDT does not result in these tissue-damaging problems. In addition, PDT is one therapeutic option for inoperable lung cancer where other options have been exhausted (5). A growing problem for lung cancer patients is airway obstructions that can manifest as intrinsic (endobronchial tumor growth), extrinsic (extrabronchial tumor compression), or mixed obstructions.
A potential to improve tumor response and survival
At present, additional treatment options and numerous hospital visits are needed to treat these patients and to improve the tumor response and survival. In contrast, endobronchial obstructions have several treatment options including surgery or heat treatments followed by airway stenting. Therapeutic options for endo/extrabronchial (mixed) tumors are currently limited and treated with stents following balloon dilation. Along with the development of interventional pulmonology, photodynamic therapy is being used in the treatment of respiratory malignant tumors because of its low level of trauma, high specificity, and compatibility with traditional or common therapies (5). Simphotek and its academic collaborators are engaged in a Phase I/IIa (NCT03735095) clinical trial to treat MCAO.
This therapy is becoming more common due to advanced primary lung cancer (6). In this trial, to treat MCAO an ultrasound system (Endobronchial Ultrasound, EBUS) is used that images the tumor and guides fiber insertions into the tumor to treat it with I-PDT. Prior to treatment a CT scan of the chest is obtained to identify the airway, the tumor, and the amount of blockage that may be present.
This is imported into Dosie by the study team to simulate treatment.
The results of simulations help to determine specific parameters for the treatment: the laser and diffusing fiber configurations. The goal is to treat the tumor’s greatest volume with the least exposure to the major blood vessels or other sensitive areas. We hope that this clinical trial will bring us one step closer to our aim of treating patients as safely and effectively as possible.
We have described a novel light-based method to treat solid cancers with fewer side effects than traditional methods.
References
- www.transparencymarketresearch.com
- www.mordorintelligence.com
- www.cancer.org
- www.globenewswire.com
- F. Jin, H.Wang, Q. Li, C. Bai, Y. Zeng, G. Lai, S. Guo, X. Gu, W. Li, H. Zhang, “Critical application of photodynamic therapy for malignant airway tumors in China”, Thorac. Cancer.2020;11(1):181–19
- https://amj.amegroups.com

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.