Given the rise in cosmetic procedures involving BoNT-A, cosmetic physician Dr Mary Dingley discusses the therapeutic implications of antibody-induced resistance on future treatment of various conditions, including post-stroke spacticity and pain disorders
Botulinum neurotoxin type A (BoNT-A) is produced by the Clostridium botulinum bacterium and is the most powerful neurotoxin known. But it is also a very useful medication. It is used to treat the symptoms of neuromuscular disorders such as cervical dystonia, cerebral palsy, post-stroke spasticity, and migraine and pain disorders. It is also a key part of the frequently used, minimally invasive cosmetic procedure called ‘BOTOX’. However, the increasing aesthetic use of BoNT-A raises concerns that this may render the substance therapeutically useless or ineffective.
Botulinum neurotoxin-A
In nature, BoNT-A enters the body via the gut (by eating contaminated food). It has a coating of accessory proteins to protect the core toxin from digestion and facilitate its passage through the gut wall. These neurotoxin-associated proteins (NAPs) take no part in the action of the core neurotoxin, the main one being the blockage of neurotransmitter release from nerves so that muscles do not contract.
Therapeutically and aesthetically, BoNT-A is injected, so there is no requirement for NAPs to be present. However, treatment results are temporary, so injections are usually repeated every three to four months to maintain the beneficial effect.
How does the immune system produce antibodies to BoNT-A?
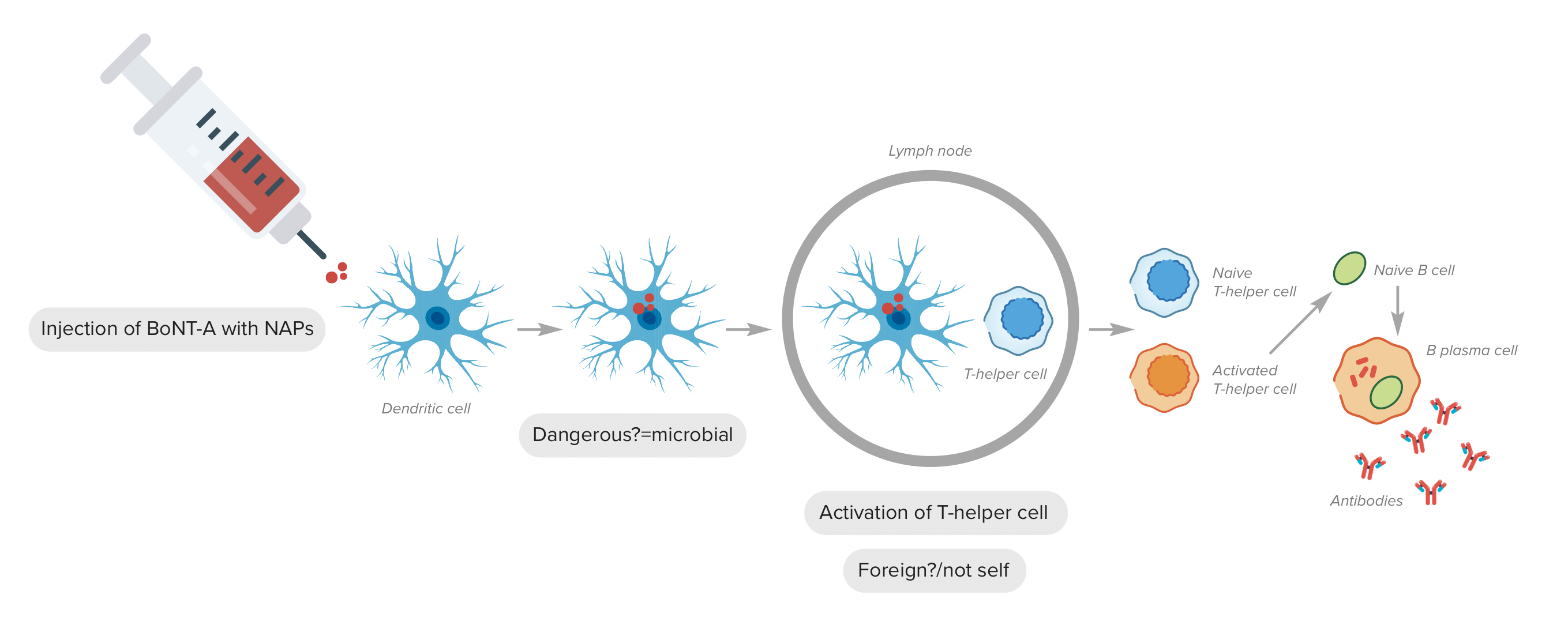
The immune system employs a two-step assessment process to make antibodies. Initially, dendritic cells decide whether substances are dangerous. For example, the NAPs and other bacterial-derived components, such as flagellin, denatured neurotoxin and clostridial DNA, are considered dangerous; however, the core neurotoxin is not deemed so (in nature, the NAPs and core neurotoxin arrive together). Secondly, at lymph nodes, dendritic cells would present the dangerous antigen to the T Helper cells, which decide whether the substance is foreign or non-self. Both NAPs and core neurotoxin are foreign, so antibodies will then be formed by the activated T cells and B cells.
If NAPs are absent, dendritic cells do not tend to ‘see’ core neurotoxin, so it does not enter the immune pathway, and antibodies are not produced. However, in the presence of NAPs and other ‘danger’ signals, BoNT-A may accidentally be gobbled up by activated dendritic cells, thereby entering the immune pathway, and antibodies may be formed.
As treatment with BoNT-A is usually ongoing, repeated injections act like booster vaccinations and further stimulate the immune system to increase the production of antibodies against BoNT-A, impairing BoNT-A’s ability to block targeted neuromuscular junctions.
What is the result of this immune stimulation?
Over time, the increase in antibodies against BoNT-A may mean treatment efficacy declines. This is usually seen as increasing dose requirements to achieve the same, or a lesser, effect and a decrease in time between treatments (dose and interval creep). This may lead to a cessation of benefit known as secondary non-response (SNR).
While immunoresistance resulting in SNR has long been recognised in therapeutic treatments, it was thought that this was not of concern in cosmetic treatments due to the lower dosages employed. However, cosmetic use has dramatically expanded, with more people having more indications treated and higher dosages being used for some of these indications. Treatment may also occur over entire adult lifespans, so it is hardly surprising that reports of immunoresistance from cosmetic exposure to BoNT-A are increasing.
While immunoresistance has been reported to occur immediately following a second BoNT-A treatment, it usually develops progressively over several years, with signs of dose and interval creep being apparent. This may be readily documented in the therapeutic world, where patients are usually treated in the same facility which records all their treatment history, but cosmetic patients may frequent different clinics and change practitioners, especially if they feel their treatments are not giving them the same results as previously obtained. This makes it much harder to follow patients’ progress accurately.
Should SNR develop through cosmetic exposure, it may mean that in later life, should BoNT-A be required for a neuromuscular concern, such as post-stroke spasticity, it will not work. BoNT-A is the only available medication choice for some of these neuromuscular disorders, leaving patients with no other treatment options.
Do all BoNT-A formulations have NAPs?
In the 1990s, the commercially available forms of BoNT-A reduced the overall bacterial protein load in their formulations. This significantly reduced the degree of immunoresistance which occurred; however, it did not eliminate it. Currently, there are more forms of BoNT-A available, but only one (incobotulinumtoxin-A) has completely removed the NAPs from its formulation. There has been no documented case of immunoresistance when this form of BoNT-A is used exclusively.
What can be done to reduce immunoresistance to botulinum neurotoxin-A?
Using the lowest effective dose and ensuring treatment doses are not administered too frequently may reduce the stimulation to the immune system. Avoiding top-up doses wherever possible may also help. It would seem prudent to use the least immunogenic form where treatment efficacy is equivalent among various forms of BoNT-A. Agencies that approve medicines worldwide may wish to look at biological medications over a longer time frame, as immunoresistance usually develops over several years.
Patients, whether having therapeutic or cosmetic treatments, should be educated and informed about which toxins are being administered to them, along with the risk of immunoresistance and its possible future implications.
References

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


