Amit Walia, Matt Shew and Craig A. Buchman from Washington University School of Medicine, explain the challenges of understanding variables or factors informing CI performance and how this can be addressed
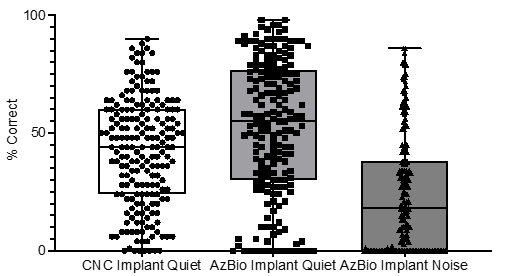
Cochlear implants (CIs) are highly effective for restoring hearing in individuals with moderate-to-profound hearing loss who do not gain sufficient benefit from hearing aids. Despite being one of modern medicine’s most successful advancements, there is wide inter-individual variability in speech perception outcomes (Figure 1). The drivers of this variability are not well understood, making it difficult to set realistic expectations for patients before surgery and to evaluate potential interventions that may enhance performance post-operatively. Accurate prediction of speech perception performance after surgery could significantly impact how we assess candidates, plan postoperative aural rehabilitation, choose surgical techniques, design and fit electrodes, and segment the patient population in future CI clinical trials.
Duration of deafness
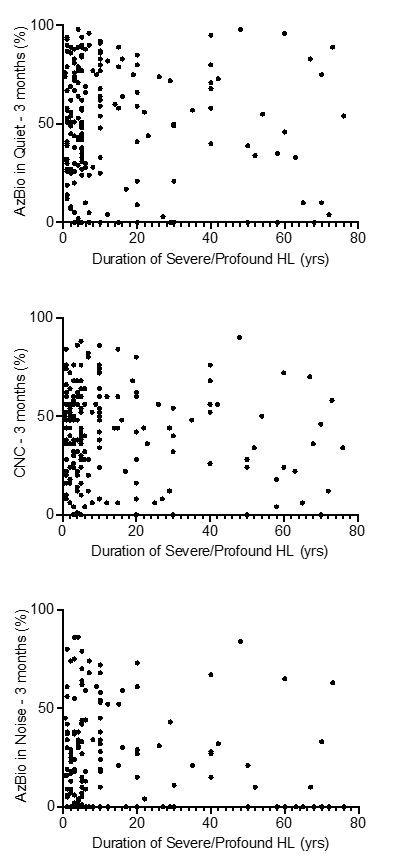
The duration of deafness has long been considered the most significant predictor of CI performance, with longer durations associated with poorer outcomes. This was especially true for patients with prelingual onset hearing loss. However, as prolonged deafness becomes less common, its predictive value has decreased. Research, including studies conducted at Washington University in St. Louis, indicates that the duration of deafness accounts for less than <20% of the variance in CI performance. (1-5)
More recent findings show almost no correlation between the duration of post-lingual deafness and CI performance (Figure 2). This is evident as patients with even >50 years of deafness can achieve excellent improvements in speech-perception performance with a CI.
Audiologic variables (preoperative evaluation)
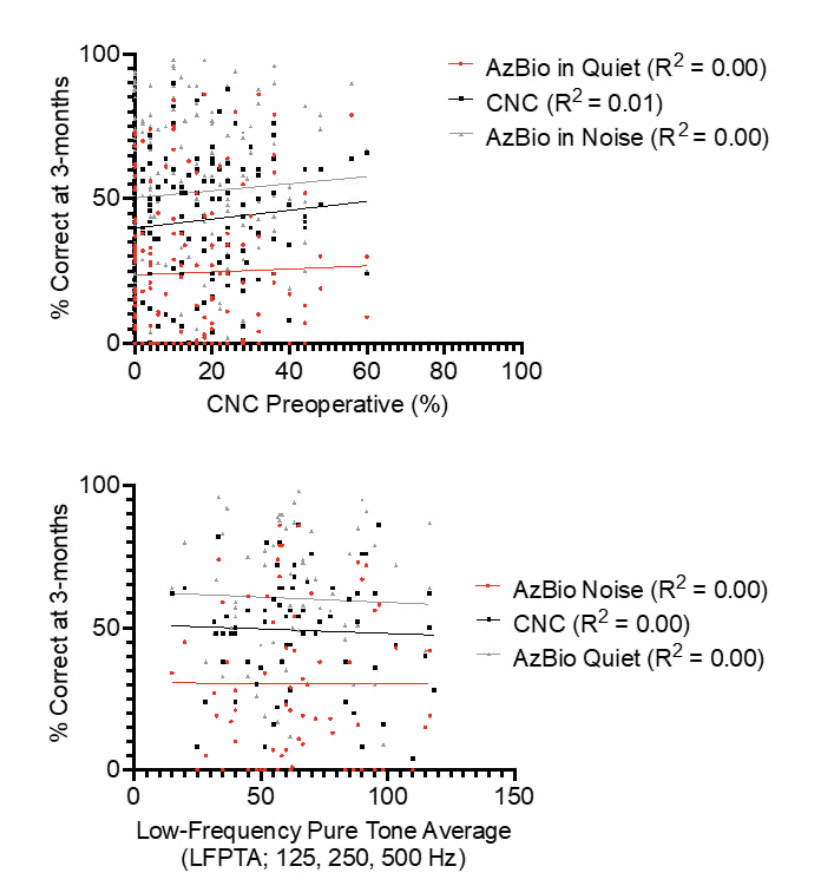
Preoperative evaluation with audiologic and speech recognition testing is essential in identifying patients who are candidates for CIs. Current data shows that while this testing can define those with poor hearing aid performance and, thus, good CI candidates, it does not predict the degree of benefit the individual will experience after CI. Conventional pure tone and speech audiometry and aided speech-perception tests using amplification (CNC words and AzBio sentences in quiet or noise) have not proven to be reliable predictors of CI performance (Figure 3). This limitation further complicates the ability to set realistic expectations and tailor interventions to individual patients.
Surgical variables
Identifying surgical variables or factors that predict CI performance is a significant challenge. There is considerable variability in the devices available, from lateral wall to peri modiolar electrodes, electrode lengths, and differing stimulation strategies. Over the past decade, some concepts in CI innovation have become clearer.
For instance, shallow insertions in the absence of hearing preservation can negatively impact performance, indicating that adequate cochlear coverage is necessary for good CI outcomes. (6) This can likely be achieved through deep or perimodiolar insertions or combined electric and acoustic stimulation in the same ear. (7-9)
However, the exact threshold or amount of coverage required remains unclear. Additionally, patients with scala tympani insertions perform better than those with scala vestibuli insertions. (1)
At Washington University in St. Louis, we have been performing postoperative CT scans on CI patients to understand the overall anatomy and location of the CI electrode. By creating 3D reconstructions augmented using a micro-CT library, we can analyze features such as angular insertion depth, perimodiolar proximity, scalar location and their potential impact on performance. Our observations suggest that shallower insertions result in worse performance in those without preserved low-frequency hearing after implantation, but the impact is limited.(3) Again, one major challenge in studying various surgical techniques or technological innovations is the inability to prognostically stratify patients. This limitation is a pervasive challenge in CI speech perception outcomes research and makes it difficult to design studies that determine the impact of specific surgical interventions on performance. This further emphasizes the importance of identifying biomarkers that can predict CI performance.
Importance of cochlear health
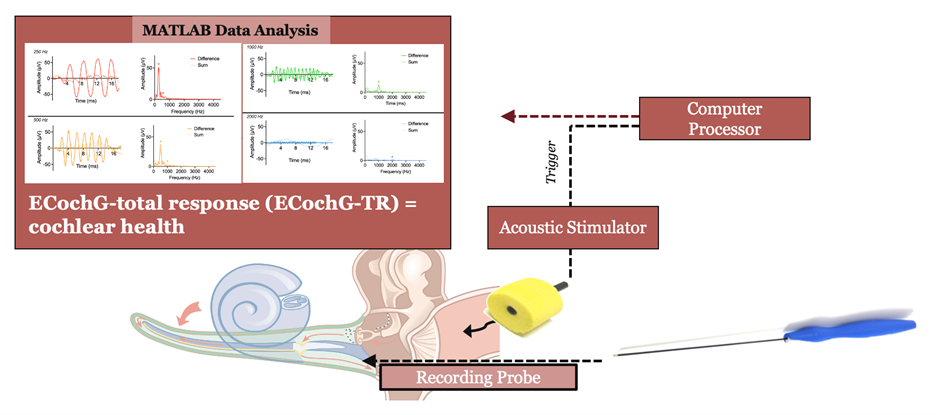
Recent literature has emphasized the importance of cochlear health and spiral ganglion survival in CI performance. (10) Essentially, better cochlear health describes a biological substrate that can be effectively stimulated with a CI. One way to assess this is through electrophysiologic recordings of the cochlea, such as electrocochleography (ECochG), in response to natural acoustic stimuli. (2-5), (11) ECochG can be performed prior to implantation to evaluate the functional status of the cochlea. Notably, ECochG responses are present in over 95% of CI recipients, even in those with ‘no- response’ audiograms and very poor word recognition scores.
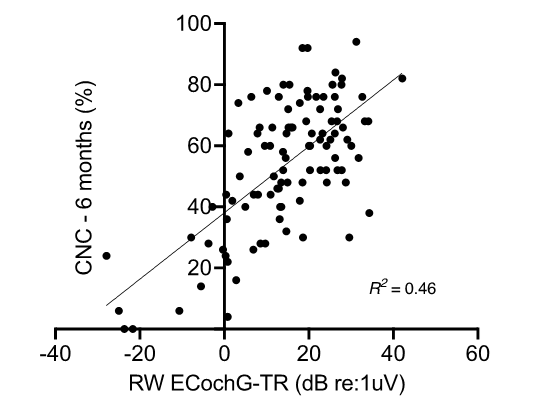
A single measure of residual cochlear function, ECochG-total response (ECochG-TR), can be calculated by summing the responses to acoustic tonal stimuli of different frequencies across the speech spectrum (Figure 4). Our research has shown that when controlling for intraoperative surgical trauma and advanced age, ECochG-TR can account for approximately 47% of the variability in speech-perception outcomes at three to six months post-implantation (Figure 5). Moreover, ECochG-TR independently explains the variance in CI performance better than the combination of demographic, audiometric, and surgical factors described above. Adding the traditional preoperative variables to ECochG-TR in a multivariable regression model does not improve the prediction of performance compared to using ECochG-TR alone. This implies that ECochG-TR integrates all these preoperative variables into a single, comprehensive measure.
References
- Holden LK, Finley CC, Firszt JB, et al. Factors affecting open-set word recognition in adults with cochlear implants. Ear Hear. May-Jun 2013;34(3):342-60. doi:https://doi.org/10.1097/AUD.0b013e3182741aa7
- Walia A, Shew MA, Kallogjeri D, et al. Electrocochleography and cognition are important predictors of speech perception outcomes in noise for cochlear implant recipients. Sci Rep. Feb 23 2022;12(1):3083. doi:https://doi.org/10.1038/s41598-022-07175-7
- Walia A, Shew MA, Lefler SM, et al. Factors Affecting Performance in Adults With Cochlear Implants: A Role for Cognition and Residual Cochlear Function. Otol Neurotol. Dec 1 2023;44(10):988-996. doi:https://doi.org/10.1097/mao.0000000000004015
- Walia A, Shew MA, Varghese J, et al. Improved Cochlear Implant Performance Estimation Using Tonotopic-Based Electrocochleography. JAMA Otolaryngol Head Neck Surg. Dec 1 2023;149(12):1120-1129. doi:https://doi.org/10.1001/jamaoto.2023.2988
- Walia A, Shew MA, Lee DS, et al. Promontory Electrocochleography Recordings to Predict Speech-Perception Performance in Cochlear Implant Recipients. Otol Neurotol. Sep 1 2022;43(8):915-923. doi:https://doi.org/10.1097/mao.0000000000003628
- Buchman CA, Dillon MT, King ER, Adunka MC, Adunka OF, Pillsbury HC. Influence of cochlear i mplant insertion depth on performance:
a prospective randomized trial. Otol Neurotol. Dec 2014;35(10):1773-9. doi:https://doi.org/10.1097/mao.0000000000000541 - Canfarotta MW, O’Connell BP, Giardina CK, et al. Relationship Between Electrocochleography, Angular Insertion Depth, and Cochlear Implant Speech Perception Outcomes. Ear Hear. July/Aug 2021;42(4):941-948. doi:https://doi.org/10.1097/aud.0000000000000985
- Pillsbury HC, 3rd, Dillon MT, Buchman CA, et al. Multicenter US Clinical Trial With an Electric-Acoustic Stimulation (EAS) System in Adults: Final Outcomes. Otol Neurotol. Mar 2018;39(3):299-305. doi:https://doi.org/10.1097/mao.0000000000001691
- Roland JT, Jr., Gantz BJ, Waltzman SB, Parkinson AJ. Long-term outcomes of cochlear implantation in patients with high-frequency hearing loss. Laryngoscope. Aug 2018;128(8):1939-1945. doi:https://doi.org/10.1002/lary.27073
- Bartholomew RA, Hoffman SE, Juliano AF, et al. On the Difficulty Predicting Word Recognition Performance After Cochlear Implantation. Otology & Neurotology. 2024;45(5):e393-e399. doi:https://doi.org/10.1097/mao.0000000000004176
- Fitzpatrick DC, Campbell AP, Choudhury B, et al. Round window electrocochleography just before cochlear implantation: relationship to word recognition outcomes in adults. Otol Neurotol. Jan 2014;35(1):64-71. doi:https://doi.org/10.1097/mao.0000000000000219

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.