Reducing clinical relapses and improving quality of life is at the heart of MS treatment; here, Tara M. DeSilva explores the benefits of remyelinating versus neuroprotective therapies for tackling MS
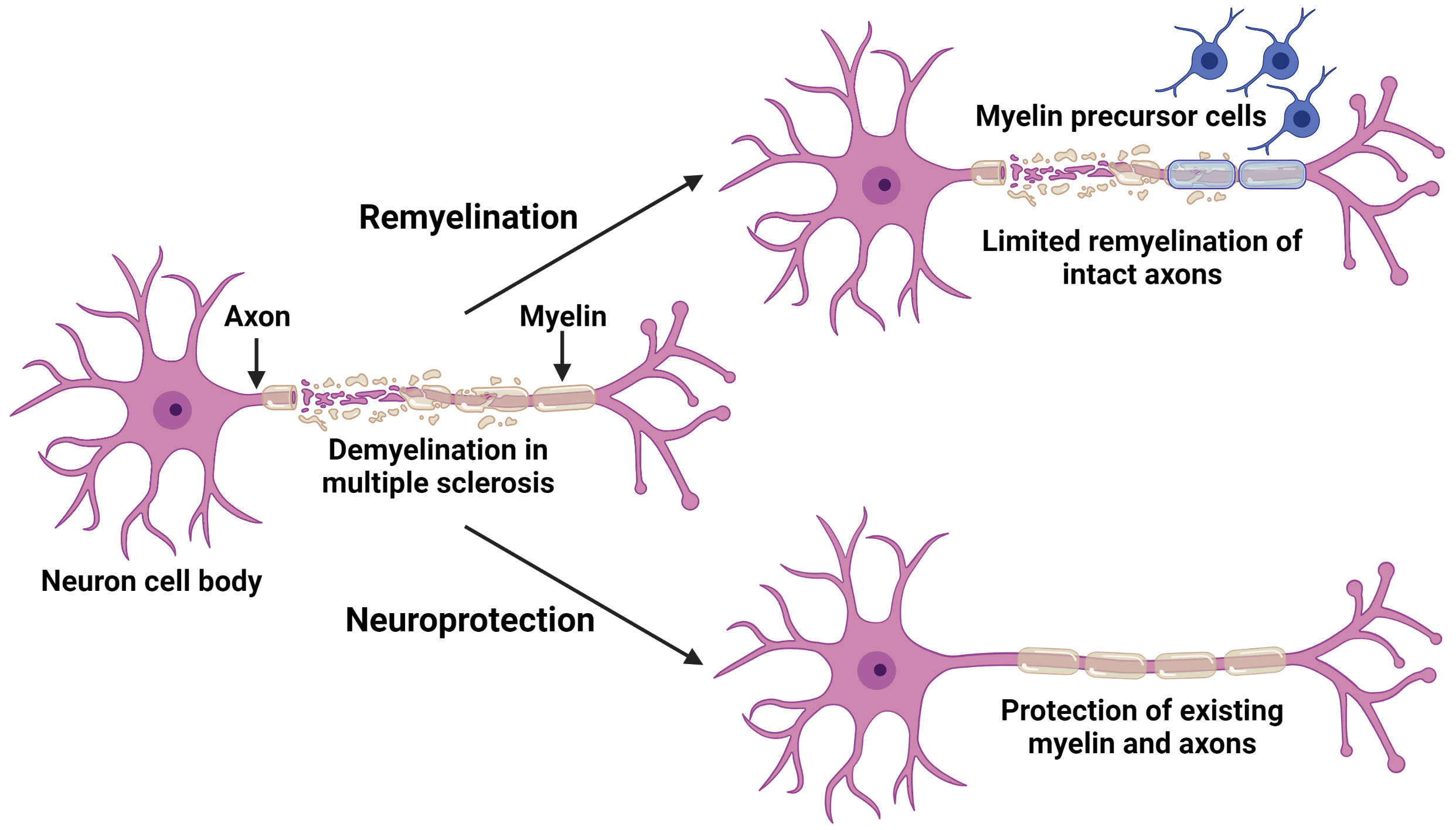
Clinical relapses in the demyelinating and neurodegenerative disease multiple sclerosis (MS) are characterised by neurological symptoms resulting from damage to the myelin sheath that surrounds axons.
This damage is perpetrated by immune cells that extravasate into the central nervous system (CNS), including the brain, spinal cord, and optic nerves and are a key underlying pathogenesis of lesion formation. Current therapies for MS reduce the infiltration of immune cells, thereby reducing clinical relapses and improving quality of life. However, inflammatory lesions in the CNS can occur even during remission leading to “silent” lesions that damage myelin and axons. This may explain why current immunomodulatory therapies are effective early in the disease course but do not prevent long-term progressive disease. Therefore, strategies are being developed to promote direct protection of the axon and recovery of the myelin sheath. These strategies, in combination with immunomodulatory therapies, may help to prevent long-term disease progression and promote recovery in MS.
Demyelination and the potential for remyelination in multiple sclerosis
Proper myelination is essential for efficient signal transduction and to protect the integrity of axons. During MS, when the myelin sheath is damaged, neuron signalling is disrupted and eventually leads to axonal injury. In an effort to repair this damage, early-stage precursors of myelin-producing cells proliferate and are present in MS lesions. When these cells mature, they can form new myelin (remyelination) to replace the areas where myelin has been lost. In MS, there is evidence of some recovery of myelin sheaths that may contribute to clinical remission. However, ongoing inflammation and scarring within the lesions prevent these cells from maturing to repair
all of the damage.
Remyelinating therapies, therefore, aim to reduce these barriers and allow more precursors to reach demyelinated axons and produce myelin to recover axons. Toward this goal, research to promote the maturation of myelin-producing cells or to reduce the inflammatory barriers to remyelination is ongoing. However, remyelinating therapies are limited to axons that are still structurally intact, as transected axons are beyond the point of repair and cannot be restored even with new myelin being produced. This emphasizes that there is a limited window of time in which an axon can be remyelinated before it begins to degenerate. Another important area of research, therefore, is to provide protection to the axon in order to prevent injury and, subsequently, the degeneration of its respective neuron cell body (i.e., neuroprotection to prevent neurodegeneration).
Axonal injury early in multiple sclerosis and developing neuroprotective strategies
Without adequate recovery, damaged axons can transect and eventually degenerate. Injured axons are observed in active and chronic active MS lesions (i.e., ongoing inflammatory activity), with the number of transected axons associated with the degree of inflammation. This suggests that axonal damage and degeneration occur early in the disease, stressing the importance of promoting repair as early as possible.
Preceding axon degeneration in MS, dysfunction of neuron signalling is known to occur. One explanation is due to the excessive production of a signalling molecule called glutamate. During MS, immune cells within the central nervous system are activated and leading to the release of excessive glutamate. This, in turn, leads to aberrant glutamate signalling not only in neurons but also to the myelin-producing cells that surround the axons, which ultimately results in cell death.
The Investigation of cell death and the protection of myelin and axons
To reduce this mechanism of cell death and investigate methods to protect myelin and axons, the DeSilva laboratory developed an in vivo model whereby myelin-producing cells are protected from glutamate-mediated damage in an established preclinical model of MS. In this study performed by the DeSilva laboratory, protecting mature myelinating cells and the sheaths they produced led to reduced clinical severity of the MS model (Evonuk et al., 2020). Furthermore, when the myelin was protected from damage, the axons underneath were also preserved (Evonuk et al., 2020). These data indicate that protecting mature myelin specifically, which is a primary target in MS, can also provide protection to the axon itself. This suggests that there is potential to provide neuroprotection even within an inflammatory environment.
MS is a complex disease, and immunomodulatory therapies cannot completely protect against myelin and axon damage.
Neurodegenerative processes begin early in the disease course, but mechanisms for repair are limited and indicate a critical unmet need for MS treatment. Two avenues, in particular, investigate strategies for recovery of the central nervous system either by promoting the formation of new myelin sheaths or by direct protection from damage altogether. A better understanding of neurodegeneration and how to protect against it will lead to neuroprotective strategies that, in combination with immunomodulatory therapies, will improve clinical care and treatment for people with MS.
Bibliography
- Evonuk, K. S., Doyle, R. E., Moseley, C. E., Thornell, I. M., Adler, K., Bingaman, A. M., Bevensee, M. O., Weaver, C. T., Min, B., & DeSilva, T. M. (2020). Reduction of AMPA receptor activity on mature oligodendrocytes attenuates loss of myelinated axons in autoimmune neuroinflammation. Sci Adv, 6(2), eaax5936.
Gabrielle Mey, a PhD student in the DeSilva Laboratory, assisted in the writing of this article

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.