Richard J Santen MD, Emeritus Professor of Medicine, Davison of Endocrinology and Metabolism, University of Virginia, Charlottesville, Virginia, U.S., charts the role of retired internists in rural, underserved communities, including diabetes telemedicine
Retired internists concept
Retired internists could markedly benefit patients by re-entering practice to co-manage patients living in rural, financially challenged, underserved areas. Telemedicine makes this feasible, and partnership with a Federally Qualified Community Health Center in the United States (U.S.) provides a practical approach. (1) Participation in such programs could allow retired internists to share their wisdom while minimizing many of the administrative hassles they previously experienced.
Background: Telemedicine for diabetes mellitus patients
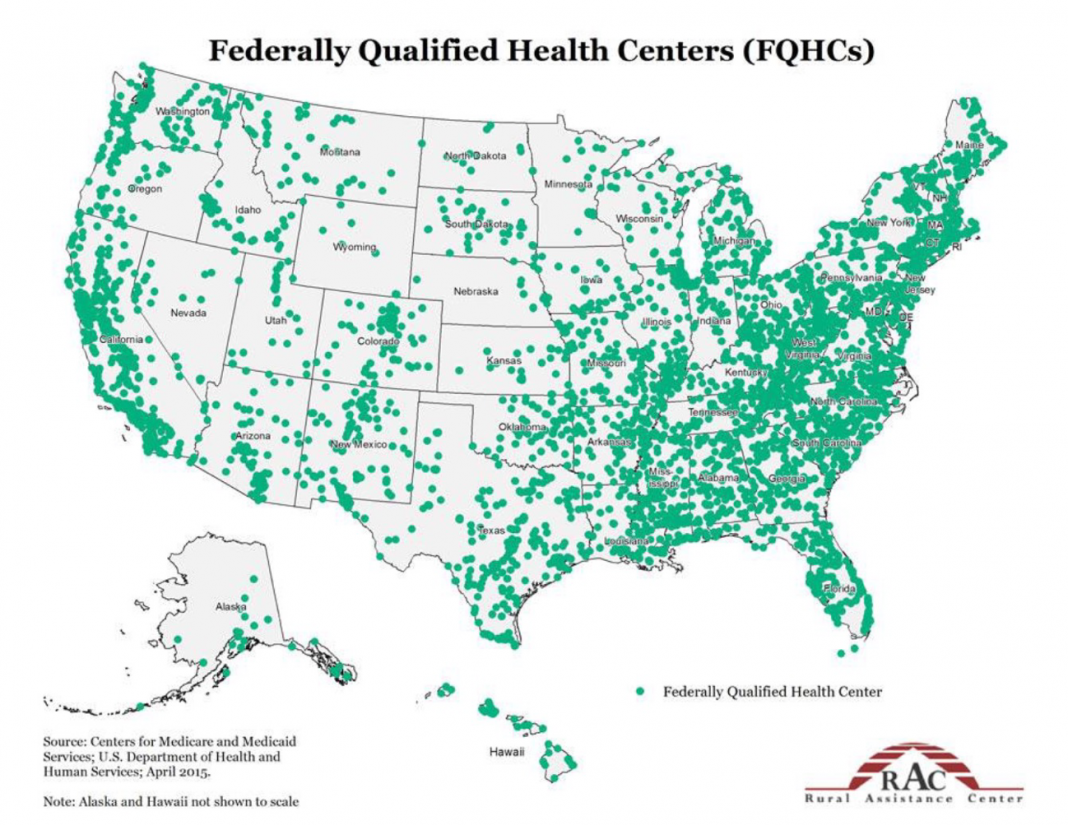
Six years ago, the author developed a program tailored to retirees that utilized telemedicine to co-manage patients with diabetes mellitus in three separate Federally Qualified Community Health Centers in rural Virginia. As shown on the map below, there are approximately 1,400 of these health clinics in the U.S. (1-2). His experience led him to the novel idea that expanding such a program nationally by convincing retired endocrinologists to return to practice via telemedicine would benefit patients and be meaningful for physicians.
A eureka moment occurred when discussing this program with his former medical school roommate, Dr William J. Hall. This approach, Hall suggested, could be effectively broadened by including both general and specialty internists and endocrinologists. Retired internists could also contribute substantially to patient management via telemedicine by re-entering practice and providing concurrent care for patients with multiple medical problems. As a result of this discussion, the idea was developed that wide dissemination of a rural-based telemedicine approach might encourage both retired endocrinologists and internists to re- enter practice on a time-limited basis.
Rationale for the idea
Wisdom is a terrible thing to waste, doubly so when it can save lives. Internists elect to retire every year when they reach a certain age, arguably when they’re still in their prime.
They benefit from wisdom gained from significant lifetime experience obtained through years of clinical practice. Many retired internists want to “give back” to society and share their wisdom and knowledge to benefit patients.
Physicians’ burnout
Recent data indicate that many physicians retire early because they are “burned out”. (3-5) The causes of burnout are many, including the hassles associated with electronic medical records, hospital regulations, long working hours, clinic time restraints, billing and coding requirements, and overly rigid hospital and government regulations.
Even in the face of burnout, retirement encourages perspective! Many physicians stepping outside the arena of a busy clinical practice often feel a sense of unfinished business or, even worse, that they are no longer needed. One solution is using telemedicine to care for patients in rural areas. Telemedicine makes it possible to manage patients at a distance. This is a golden opportunity for internists who have retired early because of burnout and those at normal retirement age who miss their interactions with patients.
These physicians can re-enter practice without the hassles, choosing how much time they would like to spend without stringent regulations. Other retired internists might be looking for additional activities after becoming bored after one to two years of retirement. They might have found that leisure time, golf, travel, and reading are insufficient to keep them enjoyably engaged.
Preliminary data supporting the hypothesis
The first author’s experience supports the feasibility of such a program. Briefly, his template involves an initial interview with patients via telemedicine, a review of the physical examination performed by the PCP (Primary Care Provider), and all available laboratory, radiologic, and clinical records. Detailed notes with specific recommendations are dictated and sent via electronically secure e-mail in PDF files to the referring provider.
Follow-up sessions are later conducted with the patient via telephone or, if necessary, telemedicine for ongoing concurrent management. A key component is to provide feedback to the referring physician. Financial rewards are minimal but sufficient to cover costs as the specialist is employed as a consultant by the FQHCs.
As a partially retired endocrinologist, Santen has co-managed more than 300 patients with diabetes in underserved rural areas in Southwest Virginia. This has resulted in significant improvement in haemoglobin A1 C levels from 10.3.±1.9% at baseline to 7.8 ±1.5% at the end of the six-month self-management period. (1)
Several important lessons emerged from this experience. One can’t just fire up a laptop and plug into a medical’ matrix.’ The staff at the rural community health centers play a pivotal role. They are, in essence, the management machine behind the whole process – they’re involved in scheduling, ordering medications and laboratory tests, non-urgent communications with patients, and coordinating consultations – this type of practice can’t be done without their input and organizational muscle.
The clinic team reduces most of the hassles of a busy clinical practice. The flexible time management strategies chosen by the internist eliminate the constraints induced by the time-dependent templates previously designed by clinic administrators.
How does one organize the process? The start-up steps can be complex for an internist to get initially involved. For this reason, a navigator (4) is helpful in handling components of the process, such as renewing the retired specialist’s medical license, obtaining malpractice insurance, purchasing dictation software, and setting up contacts with FQHCs.
A successful diabetes management program
The author has developed a detailed template for the management of patients with diabetes. His website details and illustrates his telemedicine interactions with patients and the nurse educator through a movie. This template can easily be modified for retired internists. They can then direct the management of patients with a wide range of illnesses, such as asthma, congestive heart failure, chronic obstructive pulmonary disease, angina pectoris, hypertension, obesity, chronic renal disease, and sleep apnea, among others.
More on rural diabetes telemedicine
The author has put together a website, which explains the steps necessary to get started and contains illustrative movies to illustrate the process. Further information includes blogs, published references, biographical information, and news articles. Go to this Web site to learn all about the process.
From idea to action, encourage retired internists back
This article was written with the idea that it would encourage retired internists to return to practice. They could spend the amount of time that they would like to help manage patients in their area of expertise. Action is now needed!
References
- Santen RJ, Nass R, Cunningham C, Horton C, Yue W. Intensive, telemedicine-based, self-management program for rural, underserved patients with diabetes mellitus: Re- entry of retired endocrinologists into practice. Journal of Telemedicine & Telecare.29(2):153-161.
- RJ S. Managing Patients with diabetes in rural underserved areas.
- Cunningham AT, Felter J, Smith KR, Sifri R, Arenson C, Patel A, Kelly EL. Burnout and Commitment After 18 Months of the COVID-19 Pandemic: A Follow-Up Qualitative Study with Primary Care Teams. J Am Board Fam Med. 2023;02:02.
- Hausler N, Bopp M, Hammig O. Effort-Reward Imbalance, Work-Privacy Conflict, and Burnout Among Hospital Employees. J Occup Environ Med. 2018;60(4):e183-e187.
- Scanlan JN, Still M. Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Services Research. 2019;19(1):62.
- RJ S. Need for navigators for care of patients with diabetes in rural, underserved areas. Trends Telemed E- Health. 2022;3(3):1-3.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.