Else Marit Inderberg and Sébastien Wälchli from Oslo University Hospital explore what we need to know about T cells successfully fighting cancer
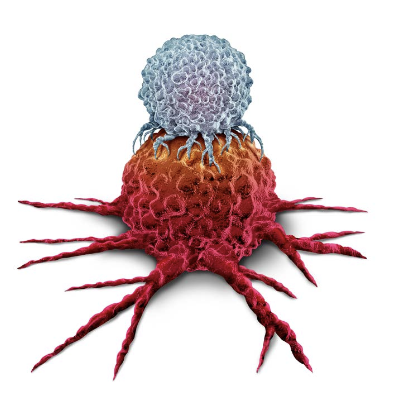
Cell-based immunotherapy uses the patient’s own immune cells to target and kill cancer cells in a specific manner. Lymphocytes called T cells are mainly used for this type of therapy, and to target them more efficiently against cancer cells, they are genetically modified to express chimeric antigen receptors (CAR) or T cell receptors (TCR) that bind proteins or peptides presented on the surface of cancer cells. There are currently six CAR T cell therapies approved for the treatment of blood cancers. However, none of these cellular therapies are yet available outside clinical studies for solid cancers.
One of the key challenges to therapeutic efficacy and availability is T cell persistence and the ability of modified T cells to penetrate solid tumours, which have numerous ways of escaping attack.
Can we grow more optimal immune cells to treat cancer?
At Oslo University Hospital, researchers are developing more efficient cell therapies. In collaboration with SINTEF, Thermo Fisher, and Oslo Cancer Cluster, a project called CellFit is currently testing ways of optimising T cell production to obtain T cells with stem-like properties. (1) The project is funded by the Research Council of Norway.
Dr Else Marit Inderberg is leading the CellFit team, which is using new technological development and robotic platforms previously exploited for drug screening. The aim is to identify chemical factors and/or novel growth mediums that will increase the proportion of efficient and persisting
T cells. The researchers then hope that their novel formula will be implemented in large-scale therapeutic T cell production.
New molecules and targeting solid cancer
In addition, the Translational Research Unit has several projects in the pipeline for developing immunotherapy and cell-based treatments more efficient in several cancers, including acute myeloid leukaemia (2) osteosarcoma (3), ovarian cancer (4), glioblastoma (5), and melanoma (6) and has recently published the first Scandinavian in-house produced TCR-based therapy. (7)
CAR molecules normally recognise proteins on the surface of cancer cells, but we have also developed several CARs that target more unconventional targets specifically expressed in solid cancers, explains Dr. Sébastien Wälchli. Some of these have finished the preclinical testing phase and are waiting to be tested in clinical trials.
First-in-human testing
Usually, genetically modified cells are changed permanently, and we infuse a “living drug” in which the modified T cells continue to divide. When testing the therapy clinically for the first time, the most important is safety. The cells should ideally not recognise healthy tissue, which may mean it is too toxic. Therefore, we have used mRNA to modify the T cells. This means that the cells only have the new receptor for a few days before it disappears, but we can give increasing doses and multiple infusions to compensate for this. If it turns out to be toxic, we can then stop the treatment, and the cells quickly lose the receptor. If the treatment proves to be safe, more permanent genetic modification can be used for later treatment.
Future development
Cell-based immunotherapies against cancer are undoubtedly here to stay and could be a valuable treatment for patients with very advanced disease. The price tag is still a challenge due to high production costs and the fact that the current therapy is produced in a personalised manner based on the patient’s own cells.
With new technological developments, these processes are becoming more automated and efficient. Important efforts are also being made to develop off-the-shelf therapies where donor cells are modified instead of the patient’s own cells, which will make the therapy much more broadly accessible.
References
- Gebhardt, T., Park, S. L. & Parish, I. A. Stem-like exhausted and memory CD8+ T cells in cancer. Nat Rev Cancer 23, 780–798 (2023).
- Caulier, B. et al. CD37 is a safe chimeric antigen receptor target to treat acute myeloid leukemia. Cell Reports Medicine 101572 (2024) doi:10.1016/j. xcrm.2024.101572.
- Mensali, N. et al. ALPL-1 is a target for chimeric antigen receptor therapy in osteosarcoma. Nat Commun 14, 3375 (2023).
- Casey, N. P. et al. Efficient CAR T cell targeting of the CA125 extracellular repeat domain of MUC16. J Immunother Cancer 12, e008179 (2024).
- Mensali, N. & Inderberg, E. M. Emerging Biomarkers for Immunotherapy in Glioblastoma. Cancers (Basel) 14, 1940 (2022).
- Dillard, P. et al. Targeting Telomerase with an HLA Class II-Restricted TCR for Cancer Immunotherapy. Mol Ther 29, 1199–1213 (2021).
- Maggadottir, S. M. et al. Transient TCR-based T cell therapy in a patient with advanced treatment-resistant MSI-high colorectal cancer. Mol Ther S1525- 0016(24)00225–9 (2024) doi: https://pubmed.ncbi.nlm.nih.gov/38582964/

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


