Ernesto Figueiro-Filho and Karolina Grzyb from the University of Saskatchewan discuss the role of placental growth factor (PlGF) in screening for preeclampsia and adverse obstetric outcomes in diabetic populations
Preeclampsia is one of the most common complications during pregnancy, affecting 2-8% of pregnancies after 20 weeks. (1) It is often asymptomatic and defined by gestational hypertension, proteinuria, and one or more adverse conditions (maternal end-organ complication or evidence of uteroplacental dysfunction). (1) Early detection of preeclampsia during routine prenatal testing is important due to the asymptomatic nature of the condition. (2, 3) The management goal of a pregnant person with preeclampsia is ultimately to monitor the maternal-fetal complications and to reach the minimum safe gestational age for delivery. (4, 5)
In the pursuit of effective prediction, diagnosis, and management of preeclampsia, recent research has unveiled novel diagnostic tools, with Placental Growth Factor (PLGF) emerging as a promising biomarker. (6, 10) PLGF, first isolated in 1991, (11) is a crucial angiogenic factor that plays a pivotal role in healthy placentas. (6, 12, 13) Dysregulation of placental development and function can lead to a myriad of complications, with preeclampsia being one of the most serious and life-threatening conditions. (9)
In an uncomplicated pregnancy, PLGF concentrations vary in each trimester, increasing from 11–12 weeks of gestation with a peak at the 30th week, after which levels gradually decrease. (4, 13, 14) Placental growth factor is considered one of the major predictors of the occurrence of adverse obstetrical outcomes during pregnancy, such as preeclampsia, fetal growth restriction (FGR), preterm birth and stillbirth. (15, 16)
Our research group at the University of Saskatchewan has collected patient data on PLGF testing since the end of 2021. The preliminary results on PLGF levels, assessed on one hundred and sixty-eight patients with indication to have the test performed, revealed that 50% of them presented borderline low, low or very low levels of PLGF, thus indicating these patients are at more risk of developing pregnancy complications. (16) For individuals with low/very low PLGF levels, our data showed the average gestational age of onset of preeclampsia at 28 weeks.
These preliminary findings suggest a potential correlation between PLGF levels and the timing of preeclampsia onset. Further analyses and a larger sample size are warranted to validate and expand upon these observations. The study aims to contribute valuable insights into the predictive values of placental growth factor levels in identifying high-risk pregnancies and optimizing clinical management strategies for preeclampsia. These results would be fundamental in planning pregnancy care in distant and rural areas, encompassing First Nations communities, one of the main characteristics of the province of Saskatchewan. (17)
Placental growth factor and diabetes
According to national statistics, approximately 8.1% of the Canadian population has diabetes (18), and like many urban centers, Regina, SK, has seen an increase in the prevalence of diabetes in recent years. Among the population of Saskatchewan, 27% live with diabetes or prediabetes and 9% live with diagnosed diabetes. (19) Indigenous populations often face a higher risk of developing type 2 diabetes compared to the general population, usually attributed to lifestyle, ethnicity, access to healthcare, and genetic predisposition. (20)
The preliminary results of our investigations showed that low/very low PLGF levels were identified in 63% of the patients with GDM, 27% of patients with type 2 DM and 10% of patients with type 1 DM (Fig. 1). Preeclampsia was found in 31.5% of all studied patients (53/168), and within this subgroup, 58.5% (31/53) had diabetes (GDM, type 1, type 2 DM). These findings demonstrated a statistically significant association between preeclampsia and diabetes (X2 (1, N = 168) = 4.0, p= 0.04).
Placental growth factor and perinatal outcomes
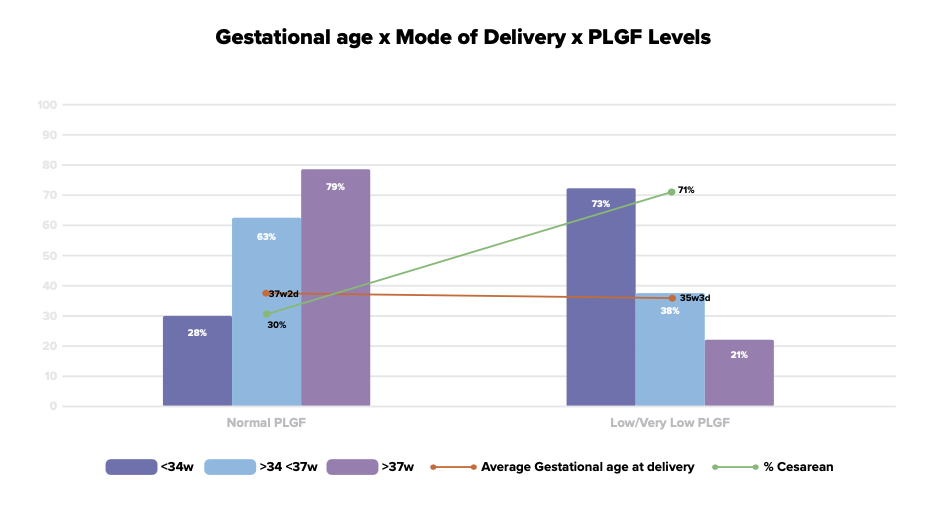
Our preliminary results also demonstrated that low/very low PLGF levels were associated with worse perinatal outcomes, specifically increased rates of preterm births (< 34 weeks of gestation), lower gestational age at delivery (approximately 35 weeks and three days) and increased rates of cesarian sections (Fig. 2). On the other hand, normal PLGF levels were associated with normal pregnancy outcomes, with no preeclampsia, no FGR, and vaginal term deliveries (> 37 weeks of gestation), with normal neonatal birthweight.
Future research on placental growth factor in Saskatchewan
Our group is continuing the research on PLGF in a population with an elevated prevalence of diabetes and was recently granted C$150,000 from Saskatchewan Health Research Foundation (SHRF) to assess local PLGF data, prospectively. Plans include a randomized clinical trial to test the hypothesis that low molecular heparin associated with aspirin in patients with low PLGF can improve pregnancy/ perinatal outcomes. (20-22) New research demonstrates that low molecular heparin used on patients with low PLGF levels may potentially augment PLGF production by the placenta. (23-25)
Moreover, our research contributes to implementing a PLGF test in the province of Saskatchewan and establishing this simple and effective test as routine for the clinical/obstetrical management of high-risk pregnancies, specifically in rural areas.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.


