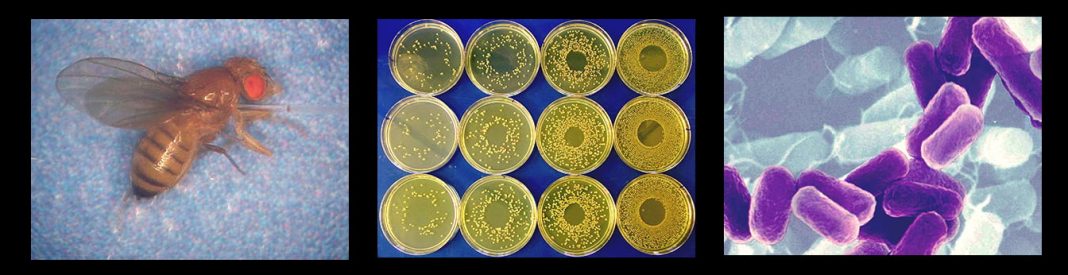
Brian P. Lazzaro from Cornell University discusses his research on the factors influencing immune response and infection outcome, drawing on powerful experimental systems, such as Drosophila melanogaster as a model host, to gain a deeper understanding of foundational biological processes
The intuition that nutrition affects immunity is as old as mothers and chicken soup. However, much more recently, we have begun to understand why and how diet and other environmental factors shape defense against infection. While we often think of the immune system as discrete, the reality is that it is interwoven with other physiological processes. As the environment affects host physiology, it also alters immune function. Furthermore, because the host is itself the habitat in which the pathogen lives, changes in host physiology are environmental changes for the pathogen. The external environment, therefore, shapes infection outcomes by altering the quality of host immune defense and through indirect effects on pathogen behavior.
Our research team studies how genetics and environment intersect to determine the outcome of opportunistic bacterial infections. These are infections from bacteria commonly present in the environment, generally causing no harm, but that can colonize a host if given the chance. Opportunistic infections impose a substantial public health burden, costing hundreds of billions of dollars per year in treatment and loss of workplace productivity. These infections typically sit at the edge of host control, where modest differences in host condition at the time of infection can mean the difference between a mild infection that is easily overcome versus a severe infection with a major health impact.
Why study infectious disease in an insect?
We do much of our work using the fruit fly Drosophila melanogaster as a model host. Core physiological and immunological processes are highly conserved across animals. For example, the fundamental elements of insulin signaling and innate immune responses are extremely similar between fruit flies and humans. We can, therefore, also expect the interaction between them to be similarly conserved, leading to shared immunological sensitivity to dietary nutrition. In addition to serving as a biomedical model, Drosophila is also a powerful model for other insects. Insects that vector human diseases such as malaria, sleeping sickness, and Lyme disease are themselves infected by the pathogens they transmit. Furthermore, pathogens and pathogen products are used in agricultural contexts for pest control. Understanding the immune defense in insects can lead to tools for improving public health and ensuring food security. The wealth of genetic tools available for working with Drosophila combines with a low cost of rearing and high experimental throughput to enable research that would not be possible in any other system. Yet the conclusions that can be drawn from this experimental model can have wide applications.
Infection outcomes are a function of host and pathogen physiology
A large body of research in humans, Drosophila, and other animals demonstrates the enormous importance of dietary nutrition on immune defense. We and others have shown that elevated dietary sugar causes hyperglycemia and leads to worsened outcomes from bacterial infection. The deterioration of immunity in individuals on high-sugar diets may partly stem from metabolic dysregulation of the immune system, including negative feedback between insulin signaling and immune signaling pathways. Adverse infection outcomes can also arise when pathogens can access the extra sugar in the blood to promote their own growth. Thus, diets high in simple sugars (such as the ‘Western’ diet) may compromise defense against infection through a dark synergism of boosting pathogen proliferation while simultaneously hampering the host immune response.
Other necessary biological processes can also compromise immune performance. For example, reproduction comes at the expense of immunity in many organisms. Mammalian females immunosuppress themselves to avoid immunological reactions against a developing fetus. Insects do not (usually) gestate their offspring internally. Still, the energy devoted to producing eggs may be drawn away from reserves that could otherwise be used to fight infection. Emphasizing the integrated nature of these physiological processes, insects use core metabolic control pathways such as insulin signaling and TOR signaling – pathways that also feed back into immune system regulation – to gauge whether their nutritional stores are adequate for egg production.
Trade-offs between reproduction and immunity are often assumed to represent an evolutionary optimization, an intentional balance between the two processes. Intriguingly, however, we have found that reproductively-induced immune suppression in Drosophila appears to arise from physiological overload. Insects use a multifunctional tissue to call the fat body for nutrient storage, production of egg yolk, and production of antibacterial peptides (AMPs) in response to infection. When a Drosophila female attempts to simultaneously produce yolk and AMPs, the fat body shows signs of stress and reduced production of all proteins. Additionally, because yolk and AMPs must be secreted from the fat body, the secretory machinery may become overburdened. We have found that the physiological overload and the concomitantly impaired production and circulation of AMPs gives the pathogen an edge, worsening infection outcomes for the host. A critical area for future study is determining whether dietary supplementation with protein and healthy lipids can reduce physiological stress and boost AMP production, restoring immunity. Extending beyond the proximate question of egg production by insects, this work addresses a more general question about how animal tissues manage simultaneous intensive demands.
Resistance versus tolerance
Direct combat of infection is not the only road to health and fitness. Plants and animals also have the means to withstand the consequences of infection, tolerating the pathogen burden at low levels. For otherwise healthy hosts, the cost of repairing minor damage from a low-grade infection may be less than the cost of a full-blown immune response to eradicate the pathogen. This is analogous to the ‘economic injury threshold’ in agriculture, where pest control is only applied if the anticipated loss in crop value is greater than the cost of applying the control. Determining when to deploy the full immune response and when to shut it down are therefore critical elements of immune system regulation.
Whereas the immune system can readily be functionally defined, potential tolerance mechanisms are much more diffuse. Processes like wound healing and detoxification come to mind easily. Still, the capacity for tolerance can also be determined long before an infection occurs and is strongly influenced by the external environment. Nutritional reserves can be a crucial determinant of how long a host can sustain health in the face of an infection, independent of and in addition to any direct effects on immune system function. Myriad additional physiological factors may contribute to host readiness to withstand infection and return to total health after the infection is resolved. Identifying these factors and their underlying genetic and environmental bases is a crucial research objective for the near-term future.
Environmental factors like nutritional availability can readily affect resistance to and tolerance of infection, and it is increasingly possible to measure indirect influences on pathogen performance within the host. However, deciphering the mechanisms underlying these effects is challenging because they emerge from complex physiological networks within the host and pathogen and from feedback between host and pathogen. The challenge is surmountable by leveraging powerful experimental systems like Drosophila to establish foundational biological principles and generate hypotheses that can be extended into other systems.