Tunde Peto, Professor of Clinical Ophthalmology at Queen’s University Belfast, describes the symptoms, causes and treatments for age-related macular degeneration and how the prevalence of the disease could be reduced
Imagine living your life without being able to see the face of your loved ones, being able to read your phone, book a show, rebook a cancelled flight, or read the labels in the supermarket. Such tasks we do without giving these much thought until suddenly, one day, we realise that we cannot do them. Age-related macular degeneration (AMD) can lead to the loss of central vision, causing sight loss or even legal blindness.
This disease is the most common cause of blindness in those over 65, (1) and while it is genetically driven in most cases, not everyone will get the disease, even if they are at risk. Its effect can be devastating, especially for those with multiple comorbidities, who have no immediate social support and for whom reading, writing, or watching television or the birds might have been the major contributor to maintaining good mental health.(2)
Recognising age-related macular degeneration in the early stages
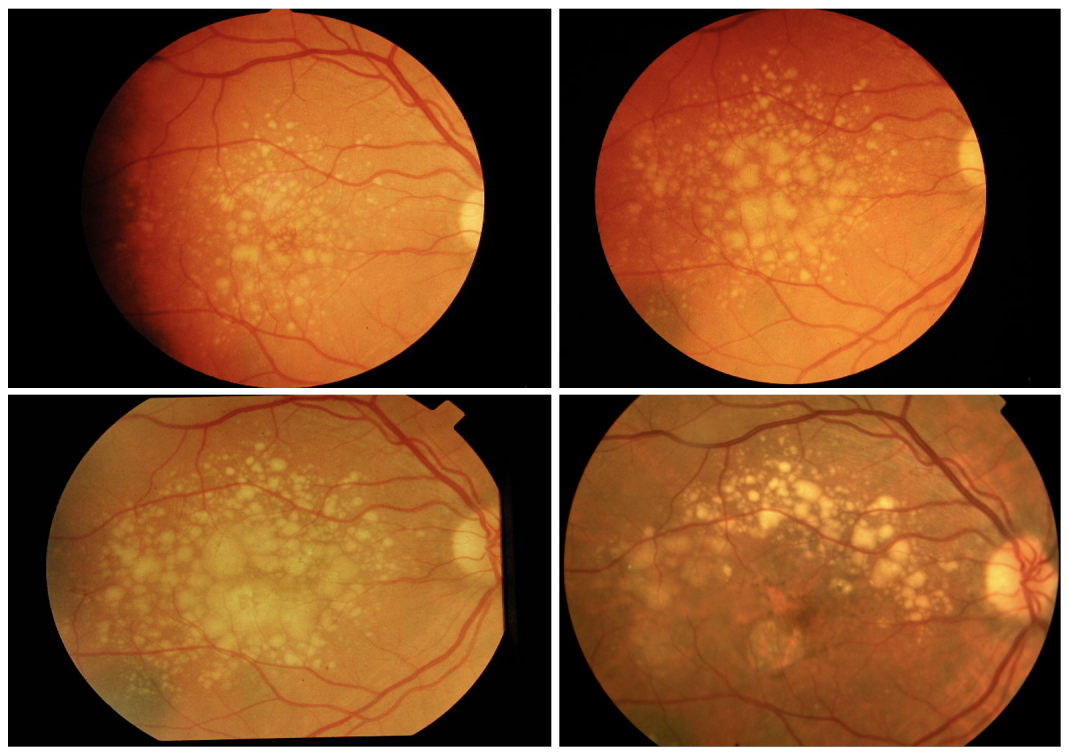
Lengyel et al. showed that age-related macular degeneration changes start early in life.(3) Some early manifestations of the disease are sub- clinical and might not even be visible when examining a person’s retina. (4) As time passes, abnormalities become more and more apparent, with small yellow deposits called Drusen appearing. These Drusen, for many individuals, have grown steadily over the years.
On the image panel, we can see the changes in the same eye that were followed for nine years. There were already large deposits at the baseline (top left-hand image). Over the years, the area and size of the deposits grew steadily before irreversible changes occurred, manifesting as the loss of cells and the development of end-stage disease (see characteristics below) accompanied by irreversible vision loss.
At the small, early Drusen stage of the disease, the central vision, as we measure it in a clinical setting, is unlikely to be affected. However, patients might complain about difficulties in seeing at dusk and dawn. Eyes with large Drusen can take a long time to recover from the incoming headlights, making the individual feel unsafe to drive. Giving up driving can lead to social isolation.(5)
Visual consequences of late-stage age-related macular degeneration
There are two significant forms of late- stage disease, commonly known as ‘wet’ and ‘dry’ AMD. (6) In the last 15 years, we have been fortunate enough to have treatment for wet AMD by direct injections into the eye.(7)
These injections have returned some lost sight or stabilised remaining vision instead of further deterioration in millions of people. The stabilised vision enabled them to live a better quality of life. Still, eventually many lose sight due to scar tissue forming and the cells dying away (atrophy).(8) The injections must be repeated regularly and place a substantial burden on the patient, their carers, society and the health system.(9)
Until recently, there was no treatment for the dry form, called geographic atrophy (GA), as the changes resemble a map. (10) GA tends to progress slowly for many patients and is unlikely to lead to vision loss as fast as wet AMD. The first promising GA treatment was approved earlier this year, and we eagerly await long-term outcomes.
Prevention, prognostication, and risk stratification
As there is no known treatment for the early disease, a lot of effort has been devoted to finding strategies to slow disease progression.(11, 12, 13) Dietary supplements are beneficial in some cases. Others have shown that a well- balanced, healthy diet throughout life will likely reduce the risk of the disease developing later in life. Smoking is one of the strongest risk factors for developing AMD; hence it is good practice to discuss stopping smoking to prevent this disease as well.
The disease affects both eyes, but for many, there is a difference in the stage of the disease, so one might be late- stage and the other one Drusen-only stage. As aforementioned, the central vision is still good for most people at the Drusen-only stage. Knowing when the second eye is likely to be affected is essential for the patient, their families and for planning clinical pathways. The EDNA study (14) showed that over three years, about a quarter of the second eyes converted to wet AMD, which is important information for those at risk and those planning clinical services for patients.
Peripheral vision and age- related macular degeneration
While the disease is called age-related macular degeneration, there is compelling evidence that the retinal periphery is also affected. (15-16) This matters to the patients as the peripheral retina helps spatial navigation and better vision in the dark. So, in addition to losing sight due to central retinal (macular) disease, patients will also have difficulties with their peripheral vision. This will result in bumping into things more often and taking longer to see in the dark. This impairs daily activities even further and can cause further anxiety and frailty.
Reducing the burden and impact of AMD
We need an even more detailed understanding of the genetic, structural, and functional changes and their interactions to categorise our patients better. This will improve targeted interventions based on individual risk profiles. We will need population-level interventions to promote good, healthy diets for all, and we need to double our efforts to keep reducing the level of smoking in the population. These, in turn, should slow the progression of the disease.
Once late disease occurs, we will need effective, affordable, safe, and long-lasting treatments. The treatment should prevent further visual loss and stop the end-stage disease from developing. Only then will we see the societal impact of this disease lessen with more older adults being able to enjoy a visually healthy life for longer.
References
-
- Wong, W. L. et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta- analysis. Lancet Glob. Health 2, e106–e116 (2014).
- Cimarolli, V. R. et al. Anxiety and depression in patients with advanced macular degeneration: current perspectives. Clin. Ophthalmol. 10, 55–63 (2016).
- Imre Lengyel, Adnan Tufail, Heba Al Hosaini, Philip Luthert, Alan C Bird, Glen Jeffery: Association of drusen deposition with choroidal intercapillary pillars in the ageing human eye, Invest Ophthalmol Vis Sci. 2004 Sep;45(9):2886-92. doi: 10.1167/iovs.03-1083. PMID: 15326099 DOI: 10.1167/iovs.03-1083
- Tan ACS, Pilgrim MG, Fearn S, Bertazzo S, Tsolaki E, Morrell AP, Li M, Messinger JD, Dolz-Marco R, Lei J, Nittala MG, Sadda SR, Lengyel I, Freund KB, Curcio CA. Calcified nodules in retinal drusen are associated with disease progression in age-related macular degeneration. Sci Transl Med. 2018 Nov 7;10(466):eaat4544. doi: 10.1126/scitranslmed.aat4544. PMID: 30404862
- De Sousa Peixoto, R., Krstic, L., Hill, S.C.L. et al. Predicting quality of life in AMD patients—insights on the new NICE classification and on a bolt-on vision dimension for the EQ-5D. Eye 35, 3333–3341 (2021). https://doi.org/10.1038/s41433-021-01414-3
- Fleckenstein, M., Keenan, T.D.L., Guymer, R.H. et al. Age- related macular degeneration. Nat Rev Dis Primers 7, 31 (2021). doi.org/10.1038/s41572-021-00265-2
- Miller, J. W. VEGF: from discovery to therapy: the Champalimaud Award Lecture. Transl. Vis. Sci. Technol. 5, 9 (2016).
- Rebecca N Evans, Barnaby C Reeves, Dawn Phillips, Katherine Alyson Muldrew, Chris Rogers, Simon P Harding, Usha Chakravarthy; IVAN Study Group: Long- term Visual Outcomes after Release from Protocol in Patients who Participated in the Inhibition of VEGF in Age-related Choroidal Neovascularisation (IVAN) Trial Ophthalmology; 2020 Sep;127(9):1191-1200. doi: 10.1016/j.ophtha.2020.03.020. Epub 2020 Mar 27. PMID: 32359843 PMCID: PMC7471837
- Kim, S., Park, S.J., Byun, S.J. et al. Incremental economic burden associated with exudative age-related macular degeneration: a population-based study. BMC Health Serv Res 19, 828 (2019). https://doi.org/10.1186/s12913-019-4666-0
- Fleckenstein, M. et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology 125, 369–390 (2018).
- Merle BMJ, Colijn JM, Cougnard-Grégoire A, de Koning- Backus APM, Delyfer MN, Kiefte-de Jong JC, Meester-Smoor M, Féart C, Verzijden T, Samieri C, Franco OH, Korobelnik JF, Klaver CCW, Delcourt C; EYE- RISK Consortium. Mediterranean Diet and Incidence of Advanced Age-Related Macular Degeneration: The EYE- RISK Consortium. Ophthalmology. 2019 Mar;126(3):381-390. doi: 10.1016/j.ophtha.2018.08.006. Epub 2018 Aug 13. PMID: 30114418
- Seddon, J. M., Willett, W. C., Speizer, F. E. & Hankinson, S. E. A prospective study of cigarette smoking and age- related macular degeneration in women. JAMA 276, 1141–1146 (1996).
- McGuinness, M. B. et al. Physical activity and age-related macular degeneration: a systematic literature review and meta-analysis. Am. J. Ophthalmol. 180, 29–38 (2017)
- Banister K, Cook JA, Scotland G, Azuara-Blanco A, Goulão B, Heimann H, et al. Non-invasive testing for early detection of neovascular macular degeneration in unaffected second eyes of older adults: EDNA diagnostic accuracy study. Health Technol Assess 2022;26(8)
- Nicola Quinn, Lajos Csincsik, Erin Flynn, Christine A Curcio, Szilard Kiss, SriniVas R Sadda, Ruth Hogg, Tunde Peto, Imre Lengyel: The clinical relevance of visualising the peripheral retina; Prog Retin Eye Res. 2019 Jan;68:83-109. doi:10.1016/j.preteyeres.2018.10.001. Epub 2018 Oct 10. PMID: 30316018 DOI: 10.1016/j.preteyeres.2018.10.001
- Lengyel I, Csutak A, Florea D, Leung I, Bird AC, Jonasson F, Peto T. A Population-Based Ultra-Widefield Digital Image Grading Study for Age-Related Macular Degeneration-Like Lesions at the Peripheral Retina. Ophthalmology. 2015 Jul;122(7):1340-7. doi: 10.1016/j.ophtha.2015.03.005. Epub 2015 Apr 11.PMID: 25870081

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.