Laneshia Conner, Assistant Professor at the University of Kentucky, discusses gaps in HIV and AIDS prevention and why greater awareness and support for HIV risk in older adults is needed
When AIDS (acquired immunodeficiency syndrome) appeared in the 1980s, blood transfusions were the route of transmission and heavily impacted older adults (those aged 50 and above).
Individuals deemed ‘at-risk’ were those who received transfusions before 1985. The social stigma surrounding HIV (human immunodeficiency virus) and AIDS as a disease primarily affecting White, homosexual males or individuals living in Sub-Saharan Africa has resulted in a lack of awareness among people outside of these groups, making it difficult for them to connect with and internalise the reality that anyone can be affected by the virus.
Clinical trials have focused on men who have sex with men (MSM), persons who inject drugs, and other sub-groups, such as ethnic minority women of reproductive age. There is a need to broaden the category of ‘high-risk’ groups to include ageing and older adults.
Ageism has increased HIV risk in older adults
While condoms provide a protective barrier from most STIs/STDs, as a form of contraception, they are not as commonly used, especially among older adults. As individuals grow older, they often encounter ageism and cultural discrimination. Unfortunately, this has put them at a greater risk of HIV transmission due to two main factors.
Firstly, they were not initially considered a population that could be affected by HIV/AIDS. Secondly, they may engage in behaviours linked to the transmission and contraction of HIV/AIDS. One of the most common HIV statistics related to age is that over half (51%) of people in the United States diagnosed with HIV were aged 50 and older and comprise nearly half (46%) of clients served by the Ryan White HIV/AIDS Program (RWHAP).
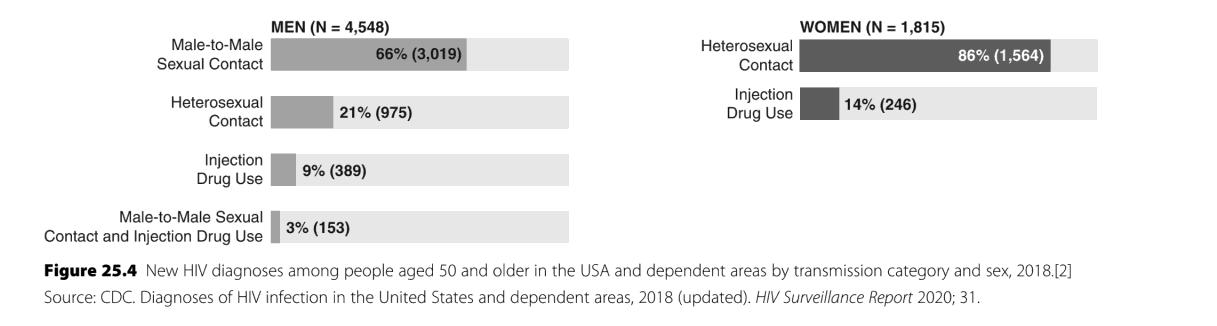
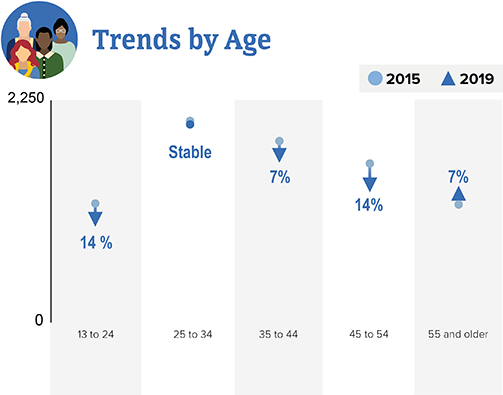
Close to half of those aged 55 and older diagnosed with HIV also had AIDS (40%), which means that they were diagnosed in the later stages of the infection. Sexual contact is the primary mode of HIV risk in older adults. According to the Centers for Disease Control and Prevention (CDC), in 2022, most of the new HIV diagnoses were among older men (N=4,548) compared to older women (N=1,815).
While HIV acquisition predominantly affects the population of men who have sex with men (MSM), increasingly, heterosexual sex has increased HIV risk among older women, especially those who belong to ethnic minority groups.
African American’s have been disproportionately affected by HIV
African American communities have been disproportionately affected by HIV, despite their smaller representation in the general population. Compared to other groups of older adults, older African Americans are at increased risk of HIV acquisition and higher rates of HIV mortality, demonstrating a racial/ethnic disparity in HIV diagnoses among adults.
Older African American males (OAAM) who have sex with males constitute 66% of new HIV diagnoses. Among older African American women (OAAW), 86% of new HIV diagnoses were transmitted via heterosexual contact.
Although older adults are receiving more attention in federally funded HIV initiatives and research, most initiatives have focused on biomedical research, neglecting important cultural and behavioural issues that influence high- risk behaviours among older adults. Accounting for relevant physiological changes can potentially address a health promotion gap for HIV risk reduction among older adults.
For example, in sexual health education, training models such as synthetic penises and vaginas are used for condom skills behavioural training and education. Most models reflect reproductive processes (i.e., a vagina for a gynaecological exam) or birth control (i.e., condom training). These popular focuses leave out the physiological changes related to age and comorbidities because their target population continues to be younger adults, particularly younger women.
Heterosexual transmission of HIV occurs through the female genital tract
Nearly 40% of heterosexual transmission of HIV occurs through the female genital tract, and there is substantial clinical evidence that supports the increased HIV risk in older adults through mucosal barriers.
In other words, a clear physiological difference exists in female and male HIV risk acquisition.
“The social stigma surrounding HIV and AIDS as a disease primarily affecting White, homosexual males or individuals living in Sub-Saharan Africa has resulted in a lack of awareness among people outside of these groups, making it difficult for them to connect with and internalise the reality that anyone can be affected by the virus. ”
Physiological changes include increased risk of contracting or transmitting HIV through vaginal sex without a condom with someone of unknown HIV status, age-related thinning and dryness of vaginal tissue, and the discontinuation of using protective barriers such as condoms due to no concern for pregnancy prevention. After menopause, there is a possibility of the vulva and vagina atrophying.
Older women also have a higher risk of developing incontinence, which can lead to vulvar and perineal dermatitis. Related to penises, the scrotum will sag, there is a loss of size, development of curvature, and erectile dysfunction, to name a few. There are additional performance-related changes due to decreased testosterone levels, nerve function, and sensitivity.
When considering comorbidities, healthcare providers should consider the physical aspect of sexual acts. Sexual health education can provide the knowledge and skills necessary to help people make safe choices and reduce misinformation; currently, it does not cater to ageing populations.
The societal norms surrounding sex have been primarily focused on non-disabled individuals and younger generations, creating a challenge for older adults. Unfortunately, sex in the later stages of life is often stigmatised as non-conventional. Increasing awareness about these important factors can greatly minimise exposure to new infections.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.