Chaith Kondragunta, CEO at AIRA Matrix Private Limited, details Artificial Intelligence-based solutions that can positively impact prostate cancer outcomes
The delivery of healthcare requires and generates large amounts of data – and thus is ripe for the application of artificial intelligence (AI) based solutions. Current AI applications in healthcare have the potential to automate routine, high-volume tasks; prioritise and triage cases to ensure patients get speedy access to the right care; and ensure that physicians don’t miss key information hidden in the large volumes of data. AI can also analyse multi-modality information to predict disease progression and treatment outcomes – a capability that is hard for the human practitioner. This predictive power of AI can play a crucial role in the cancer care pathway and impact treatment decisions and healthcare outcomes.
AIRA Matrix provides AI-driven solutions to aid predictive medicine, precision diagnostics and personalised healthcare. Our solutions for prostate cancer help in effective risk stratification of patients at the outset, and ensure that morbidity and mortality due to over and under-diagnosis of prostate cancer are reduced.
Impacting prostate cancer outcomes
Prostate cancer exhibits a broad spectrum in patients – ranging from indolent (needing only watchful waiting) to aggressive (needing immediate therapeutic intervention). Just like under/ missed diagnosis can lead to increased mortality due to the disease, over-diagnosis can lead to unnecessary treatments that can result in adverse effects like erectile dysfunction and urinary incontinence, and affect the quality of life.
For effective treatment of prostate cancer, accurate disease stratification and tailored therapy decisions are as important as early disease detection and diagnosis. Unfortunately, in current practice, early detection of prostate cancer is well-established, but early discrimination is not. At AIRA Matrix, we aim to positively impact prostate cancer outcomes by applying AI-based solutions across the care pathway – from screening to post-surgical follow-ups. These solutions not only help in accurate risk stratification, but also help the physician visualise the course of the disease and effectively tailor treatment.
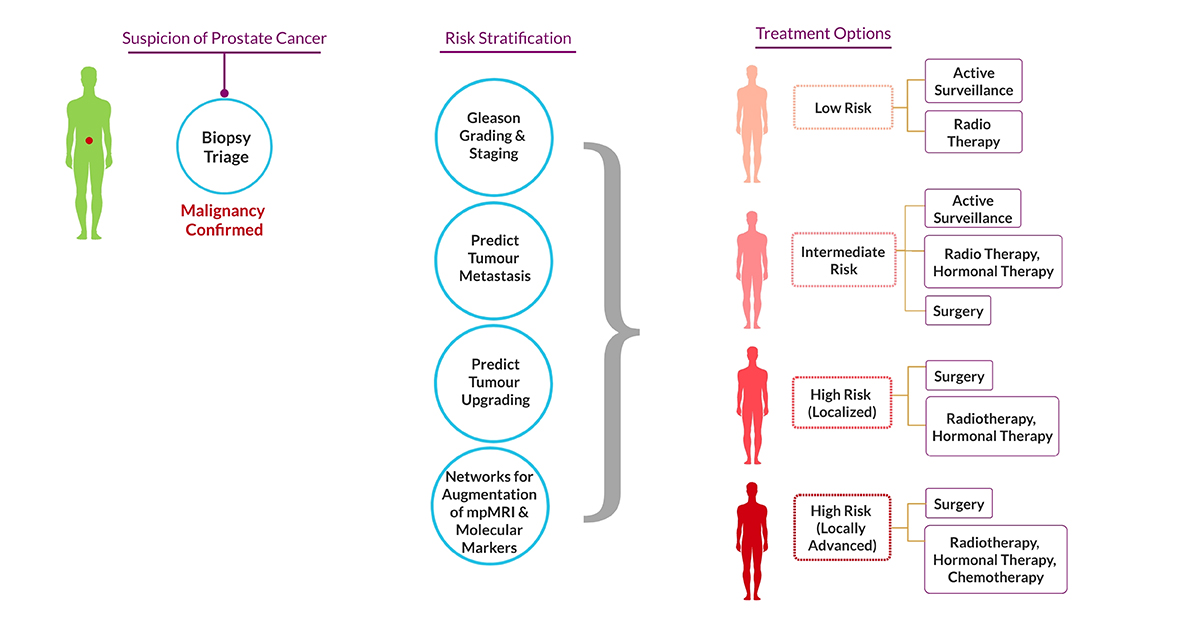
The prostate cancer care pathway broadly spans the following:
- Screening: Biopsy and other investigations for early disease detection and diagnosis.
- Stratification: Disease grading and staging using biochemical, radiological and histopathological parameters.
- Prognostication: Decisions around therapy options like watchful waiting, active surveillance, radical surgical intervention, chemotherapy, radiotherapy.
- Follow-up: Careful follow up of treated patients grouped into the above different regimen groups.
Our AI-based products and solutions act at every step of the prostate cancer care pathway:
1. Screening
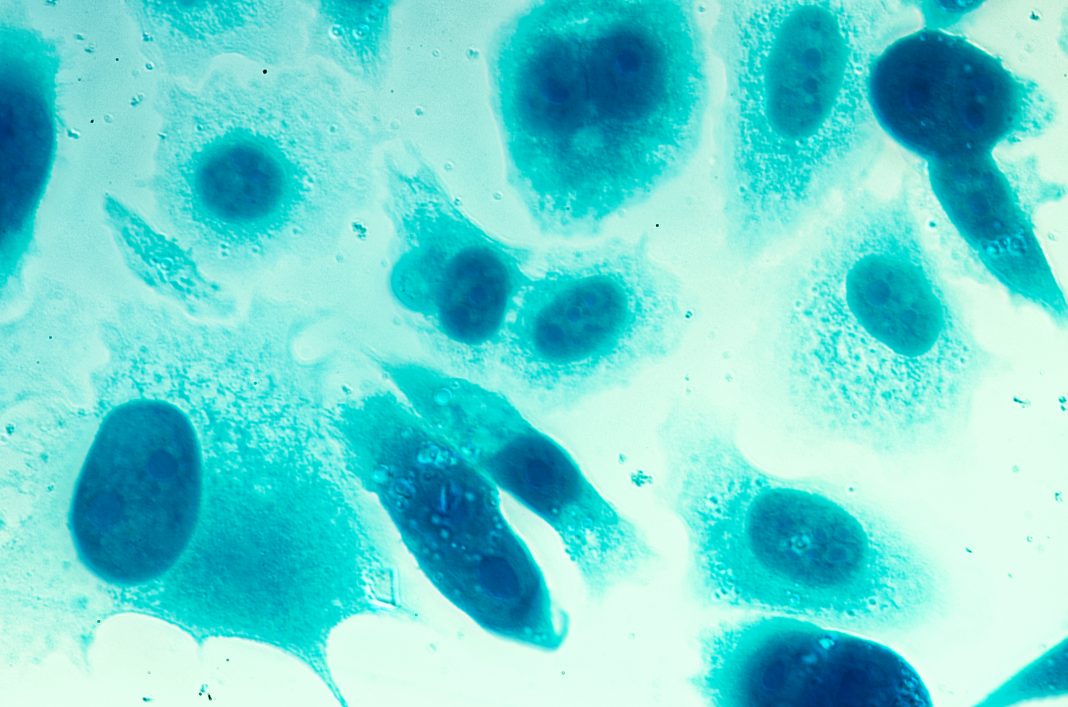
a) Our AI-based triaging solution helps in the rapid screening of prostate core needle biopsies (CNBs) to detect and diagnose malignancy. This algorithm can act in a twofold manner – by screening and triaging biopsy sections to highlight critical areas; or as a second read to identify tumour areas that may have been overlooked by the pathologist.
b) The larger increase in the number of CNBs reviewed per case over the past decade has resulted in an increased workload on the pathologist potentially resulting in delayed cancer diagnoses and possible diagnostic errors with pathologist fatigue and burnout being key contributors to these errors.
c) Our solution eases out this burden on the pathologist resulting in rapid and accurate screening and diagnoses.
2. Stratification
a) The Gleason grading system is the most commonly applied histopath-ological risk stratification method for prostate carcinoma. However, it suffers from significant inter and intra-observer variability, with a chance of under-grading in a significant number of patients.
b) Our Gleason grading solution offers high intraclass and less inter-class variation in histopathology images leading to improved accuracy, precision and speed of Gleason’s scoring.
c) Moreover, our solution uses a unique gland level grading approach, imitating the process of manual reporting by the pathologist.
d) This ensures visually interpretable results in the form of annotations and heat maps, with results that are reproducible and visually interpretable.
With an AUC of 98% for cancer detection, 96% for Gleason’s grading and 92% for ISUP grading, our solutions enable accurate, faster detection and risk stratification of prostate cancer to help guide the oncologist for confident selection of appropriate therapy regimens.
3. Prognosis
a) We are developing solutions that predict the course, spread and aggressiveness of the cancer. Our goal is to improve prognostication, therapy planning and follow up of prostate cancers – with better outcomes for the patient as well as the caregivers.
b) Our AI-based algorithms trained on long-term multimodality data (including clinical, biochemical, histopathological, radiological and molecular data) can help separate aggressive tumours that can upgrade and metastasize from tumours that will follow an indolent course.
c) Another solution is a DL network that can accurately predict bio-marker expression on routinely stained histopathology slides, without the need for expensive, time and tissue consuming molecular techniques. This translates into faster prediction of prognostic and predictive biomarker expression on lesser tissue sample, thus optimising the diagnostic pathway.
Novel solutions
In addition to the above, we are applying Artificial Intelligence to develop solutions that utilise information from the histopathology gold standard to augment other non-invasive modalities like radiology and molecular testing.
For example: Multi-parametric Magnetic Resonance Imaging (mpMRI) is currently used in primary diagnosis, risk stratification and therapy of prostate cancer patients. However, mpMRI has the following drawbacks:
a) It substantially underestimates size, extent and tumour volumes in comparison with histopathology.
b) As in Gleason grading, the accuracy of tumour detection on mpMRI is dependent on the expertise of the reporting radiologist.
To mitigate these drawbacks:
a) Our solutions provide the 3D reconstruction of tumour specimens by co-registration of mpMRI and radical prostatectomy images.
b) They provide improved tumour localisation and tumour volume detection on mpMRI, and help improve staging, focal therapy planning and follow ups.
For the patient this means accurate tumour volume estimation by non-invasive methods, with reduction in ensuing morbidity, while for the care-giver this means optimised workflows with improved staging and therapy planning, ultimately resulting in better outcomes of the patient care pathway.
Our range of solutions are developed in collaboration with leading Oncology hospitals, radiology institutes and prostate cancer research organisations across the globe. We continue to expand the focus areas of applications and actively look to partner with fellow participants in this journey.