Frédéric Destrebecq, Executive Director, and Vinciane Quoidbach, Public Health and Policy Project Manager at the European Brain Council, explain the socio-economic impact of interventions and the importance of early diagnosis with regard to brain disorders…
Depression, stroke, dementia, alcohol dependence, schizophrenia or anxiety will affect at least one in three European citizens during their lifetime – currently 165 million people in Europe (estimated 38.2% of the EU population annually)1. Brain disorders are highly prevalent medical conditions, being the seat of many chronic disabling diseases2: today, mental disorders and other brain disorders represent 35% of the burden of all diseases in Europe3. Out of 10 individuals with a brain disorder, from 3 to 8 remain untreated although effective treatments exist4. And the burden of diseases is increasing.
The relentless demand for healthcare services is set to continue for the foreseeable future, fuelled by population growth and increased longevity. However, since 2010, health systems reforms in Europe are calling for more with high societal value. A key policy driver, therefore, is the need to look at the outcomes or health benefits and to optimise healthcare service delivery (with high-quality standards, better use of resources and interaction). This is particularly challenging for brain disorders considering the management of long-term conditions including co-morbidities and occurrence of acute episodes.
From the patient perspective, early detection and diagnosis are unnecessary pain and suffering. Early diagnosis and treatment make not only clinical but also economic sense. Diagnostic testing is an integral part of the healthcare system, providing essential information to enable providers and patients to make the right clinical decisions. Indeed, some 75% of clinical decisions are based on a diagnostic test5. Demand for access to quicker, more accurate diagnosis is rising. Making detection more efficient, timely and accurate will contribute to generate the savings required by health systems.
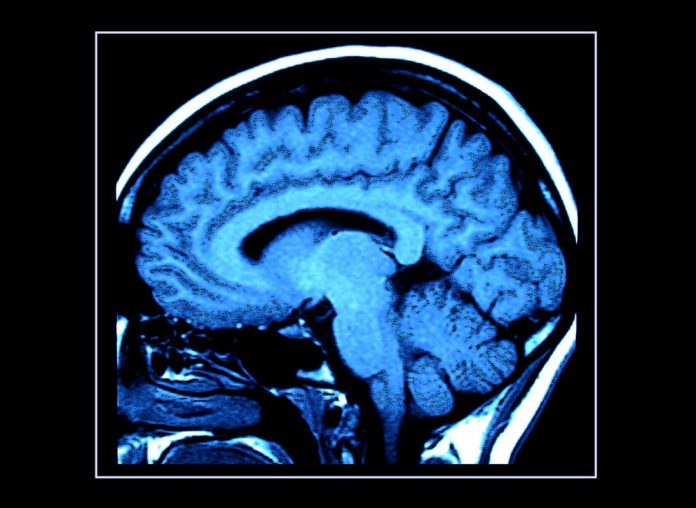
Improved diagnosis can also reduce the scale and cost of treatment. For instance, computed tomography (CT) and magnetic resonance imaging (MRI) have revolutionised the study of the brain by allowing healthcare practitioners and researchers to look at the brain noninvasively. These diagnostic imaging techniques evaluate the brain structure, allowing healthcare providers to infer causes of abnormal function due to different diseases. A large body of research links early diagnosis to measurable health gains, such as improved survival rates and lower treatment costs. However, effective implementation of early diagnosis and treatment varies widely across health systems and many European countries are still lagging severely behind.
Therefore, the following questions are raised to examine the best options to improve patients’ quality of life and reduce the socio-economic burden: what is the amplitude of current unmet needs (obstacles such as misdiagnosis, delayed treatment, affordable access to care and pricing) in health care in Europe, not only within the provision of medicines but also within health care systems and services? What is the socio-economic impact of targeting these gaps? What are the potential benefits for integrated, coordinated care combining effective team care and care planning? What are the new research developments? A large number of reviews highlight that health systems can respond to the burden of brain disorders by implementing proven, cost-effective interventions. It has proved essential to put scientific evidence into care standards.
More research evidence to develop better prevention and treatment options definitely appear to be necessary, such as :
– The availability of biological markers (biomarkers) for early disease diagnosis will impact the management of Alzheimer’s Disease in several dimensions; it will 1) help to capture high-risk individuals before symptoms develop, a stage where prevention efforts might be expected to have their greatest impact; 2) provide a measure of disease progression that can be evaluated objectively.
– Treat early and effectively new treatment paradigm: early diagnosis and disease-modifying treatments (DMTs) at the early stage of the disease to slow down the progression rate are available to manage a relapse – remitting multiple sclerosis.
In this context, the EBC Research Project on the Value of Treatment for Brain Disorders (2015-2017) is exploring through case studies analysis the potentials for early diagnosis and new treatment paradigm, generating evidence on the socio-economic benefits of healthcare (pharmacological and psychosocial) interventions, and assessing optimal strategies such as integrated, seamless care to close the treatment gap in Europe.
Value of treatment research project: Objectives and vision towards policy development
The Value of Treatment research project draws from the EBC Report “The Economic Cost of Brain Disorders in Europe” published in 2005 (Balak and Elmaci 2007) and updated in 2010 (Gustavsson et al. 2011) that provided a solid estimation of the costs of brain disorders at around €800bn per year in Europe.
In order to use data to inform policy recommendations, case studies analysis will be conducted for the following disorders: mental illness comorbidity, schizophrenia, dementia, idiopathic normal-pressure hydrocephalus, AF-related stroke, Parkinson’s disease, epilepsy, headache, multiple sclerosis, and restless legs syndrome. Scientific publications with detailed outcomes of each individual case study will also be released in the course of 2017.
The vision is clear: mental and neurological disorders, or “disorders of the brain”6 are complex and interlinked with hundreds of specific diagnosis, codified in diagnostic classifications systems (WHO International Classification of Diseases, ICD-107 and American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, DSM-V8). Although brain disorders were until recently associated with disciplinary fragmentation in research and practice using different concepts and approaches, there is today greater awareness on their burden and challenges to manage them, and even to prevent some of them (modifiable risk factors reduction), emphasising the need for developing an EU-wide Plan to address brain health in a comprehensive and collaborative way9.
1. A. Gustavsson et al. The economic cost of brain disorders in Europe, Journal of Neurology 2012.
2 H.U Witchen et al. The size and burden of mental disorders and other disorders of the brain in Europe, ECNP/EBC Report 2011.
J. Olesen et al. European Journal of Neurology 2012. 4 EBC poster « mind the gap » presented at EFNA annual conference, July 2016.
5 E. Abram et al. Screening and Diagnostic Tests. Medscape, December 2015.
6 P.Y. Collins et al. Grand challenges in global mental health. NIH. Nature ; 475(7354) :27-30. Doi :10.1038/475027a. 2011.
7 The WHO International Classification of Diseases « ICD-10 » is the standard diagnostic tool for epidemiology, health management and clinical purpose. ICD chapter V focuses on « mental and behavioural disorders » and consists of 10 main groups. WHO is revising their classifications as part of the ICD-11 (revision of the 10th edition due by 2017). With regard to neurological disorders, ICD chapter VI focuses on « diseases of the nervous system ».
8 The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) is the 2013 update to the American Psychiatric Association’s (APA) classification and diagnostic tool.
9 EBC Call to Action launched in 2015, advocating for the development of National Brain Plans (NBP) to reduce the burden of diseases and disabilities under the umbrella of an EU-wide plan addressing brain health and covering the whole spectrum of care from surveillance (patient registries) to prevention, care and support, access to treatment, evaluation and research.
Frédéric Destrebecq & Vinciane Quoidbach
Executive Director & Public Health and Policy Project Manager
Value of Treatment Research Project
European Brain Council
www.braincouncil.eu
www.twitter.com/EU_Brain