Cecilia Van Cauwenberghe from Frost & Sullivan’s TechCasting Group, explains how the COVID-19 pandemic is the scenario for testing and demonstrating the successful implementation of diabetes telehealth platforms
Considered a leading chronic disease worldwide by the World Health Organization (WHO), diabetes mellitus represents a critical health concern worldwide. Indeed, effective access to the proper care of diabetes patients differs extensively in the light of diverse factors, mostly geographic and socioeconomic. During the past five years, and especially since the start of the COVID-19 pandemic, the use of medical technology has served to significantly expand healthcare options to lower barriers and improve access for a greater number of patients. The role of telehealth in improving access to diabetes care has been remarkable (Appuswamy and Desimone, 2020). Several feasible and effective telehealth programmes to help assess and manage diabetes have been widely adopted by patients and healthcare providers. Diabetes telehealth platforms have adapted to enhance disease management, increase efficiency, facilitate clinical decision-making, and promote patient self-management skills. Diabetes telehealth platforms deployment has significantly reduced healthcare costs, sometimes reducing inequalities in diabetes care access.
Engaging patients with technology and self-management
Furthermore, diabetes telehealth platforms have successfully been used in the care of diabetes-related foot disease (DFD), microvascular complications, mental health support (Kompala and Neinstein, 2021). A wide series of digital health connected devices are arising to provide support for patients with diabetes on a daily management basis while facilitating data interoperability and integration. Diabetes telehealth platforms deliver an opportunity to increase access to continuous glucose monitoring (CGM) for patient self-management (Gal et al., 2020).
Telehealth also serves to improve training for the initiation of CGM by advising patients about the right use of easily inserted, factory-calibrated sensors, for easy platform deployment and intervention through the identification of trends and potential adjustments. Data can be shared for consultation between programmed medical visits.
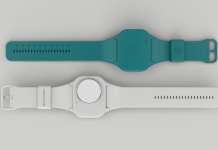
An important complication of diabetes concerns diabetes-related foot disease (DFD), which derives from foot ulcers, skin infections and potential gangrene. The risk of recurrence and complications are high, so that different types of sensors, wearables and telehealth devices have been proposed to prevent DFD complications. These systems can monitor foot temperature, plantar pressures, glucose, blood pressure and lipid levels (Golledge et al., 2020). Similarly, contact lenses and smart glasses to measure ocular pressure are being developed and as such, are proposed for diabetes telehealth platforms.
Monitoring risk factors associated with diabetes
The monitoring of risk factors associated with diabetes mellitus, including CGM, DFD, glaucoma, high blood pressure, by implementing diabetes telehealth platforms and introducing different monitoring devices has demonstrated great promise during the COVID-19 pandemic, along with telehealth consultations (Yarbrough, 2020). This patient-centric approach also serves to train patients in the correct use of devices and encourages self-management actions. Beyond conventional monitoring levels of metabolites and biomarkers, wearables can help to assess sensation, peripheral perfusion, Chemosensory Perception, among other variables of interest, through the introduction of artificial intelligence and machine learning (AI/ML) systems. For instance, gait-enhancing mechatronic systems (GEMS) have proved to improve gait and redistribute foot pressure; vascular early warning systems (VEWS) use infrared optical sensors placed on a different part of the foot to detect changes in blood volume within the microvasculature.
Sensors, wearables and telehealth approaches allow remote monitoring of the key risk factors associated with diabetes care. The COVID-19 pandemic provides a large-scale, global scenario for the testing and demonstration of the relevancy of the introduction of such innovative technological approaches for preventing complications while being safe by staying at home.
Acknowledgements
I would like to thank all contributors from industry involved with the development and delivery of this article from Frost & Sullivan.
Further reading
- Appuswamy, A.V. and Desimone, M.E., 2020. Managing diabetes in hard to reach populations: a review of telehealth interventions. Current Diabetes Reports, 20, pp.1-10.
- Gal, R.L., Cohen, N.J., Kruger, D., Beck, R.W., Bergenstal, R.M., Calhoun, P., Cushman, T., Haban, A., Hood, K., Johnson, M.L. and McArthur, T., 2020. Diabetes Telehealth Solutions: Improving Self-Management Through Remote Initiation of Continuous Glucose Monitoring. Journal of the Endocrine Society, 4(9), p.bvaa076.
- Golledge, J., Fernando, M., Lazzarini, P., Najafi, B. and G Armstrong, D., 2020. The potential role of sensors, wearables and telehealth in the remote management of diabetes-related foot disease. Sensors, 20(16), p.4527.
- Kompala, T. and Neinstein, A.B., 2021. Telehealth in type 1 diabetes. Current Opinion in Endocrinology, Diabetes and Obesity, 28(1), pp.21-29.
- Yarbrough, C., 2020. Important Changes that May Affect Telehealth Policy During the COVID-19 Pandemic. Diabetes Technology & Therapeutics.